What’s going on with the ‘magic’ drug for malaria?
Lately, Dr. Ruth Namazzi and her colleagues have been stopping one another in their hospital ward with worried looks.
Between treating patients, she says, they voice their concerns: “‘Malaria’s very stubborn,'” she says they tell her. “‘It’s not responding to treatment.'”
Namazzi is a pediatrician at Mulago Hospital in Uganda, where — several times a day — she admits a child with severe malaria.
“These are very critically ill children,” she says, explaining that children are at greater risk of severe malaria than adults because they have not yet gained immunity. Severe malaria in a child can involve a high fever, convulsions, anemia, kidney damage and respiratory distress, among other issues. “A child can become extremely weak. They can’t stand or feed on their own.”
For years, Namazzi — who is also a lecturer at Makerere University College of Health Sciences — has turned to a medication called artemisinin. The drug is derived from an ancient Chinese malaria treatment that was rediscovered several decades ago and has saved millions of lives. It made such a profound difference that one of the people who helped revive the medical recipe received a Nobel prize for her work.
“It works like magic,” says Namazzi. “Parasite clearance was very fast [compared to other malaria medications]. It had less complications. The mortality was lower.”
Is the ‘magic’ is fading?
But lately, that magic hasn’t been working so well.
After an infected mosquito bites you and deposits the malaria parasite into your body, the parasite starts to replicate. That’s where artemisinin comes in. Given intravenously at regular intervals, it can kill most of the parasites in a patient’s blood within hours. But now, Namazzi has been seeing patients where the drug takes several days to work.
She wanted to understand what was going on. So she teamed up with others to figure it out. They had several hypotheses: Maybe the dose is too small or perhaps the patients aren’t completing the full medication course.
But it was something else entirely — a worrisome new twist.
Between 2021 and 2022 in Jinja, Uganda, the researchers studied 100 kids with severe malaria, closely monitoring their mediation intake and regularly evaluating the parasite load in their blood.
“What we found was that children with severe malaria do have evidence of drug resistance,” says Dr. Chandy John, director of Indiana University School of Medicine’s Ryan White Center for Infectious Diseases and Global Health and a co-author on the study, which was published on Thursday in the medical journal JAMA. “The reason this is important is because those children with severe malaria are at the highest risk for death.”
Malaria kills more than half a million people each year, most of them are young children in Africa. This study is the first time researchers have documented signs of resistance in African children with severe malaria. It’s estimated that between one and five million children in Africa get severe malaria each year, says John. Unlike patients with uncomplicated malaria, these children have few other options for malaria drugs.
“Clinically, this is very concerning because there’s still a lot of malaria in Africa,” says Kasturi Haldar, a professor of biological sciences at the University of Notre Dame who has studied malaria for decades and was not involved in this study.
Three worries
As the study authors pored over the findings, three things concerned them: First, they found that for 11 of the 100 children it took longer than normal — more than 5 hours — for artemisinin to kill at least half the parasites in the bloodstream. These kids are considered to have partial drug resistance, under the World Health Organization’s definition. (It’s not complete resistance because the kids did eventually get better.) “Think about it, for any infection, more than 10 out of 100 people you treat don’t get better [quickly]. That’s really pretty bad,” says Haldar.
Time matters since “the longer you have a high parasite load, the more likely you are to have bad outcomes — and that’s death but it’s also other complications,” says John. “Survivors [of severe malaria] can have long-term effects. About 25% of them get neurodevelopmental impairment. And we’re also looking now at kidney injury.”
Second, the researchers found that some of the children were infected with a malaria parasite that had mutated; the altered gene they found in this parasite is associated with resistance to malaria medications.
Finally, on top of all this, the researchers found signs of resistance to an oral antimalarial drug kids are often sent home with: artemether lumefantrine. The drug is supposed to help make sure there are no remaining parasites in the body. But about 10% of the patients that doctors thought were better showed up sick again, within a month.
“So the combination [of drugs] is supposed to get rid of malaria, but we didn’t actually completely get rid of it,” says John. He says this is an indication that the parasite may be developing resistance to artemether lumefantrine too.
While all of this has experts concerned, they say it is not entirely surprising.
Resistance to artemisinin has been seen before. And it makes sense: Diseases evolve to evade drugs. In the past couple years, studies in East Africa have shown partial resistance to artemisinin in children with uncomplicated malaria. Plus, “this is quite similar to what has happened in Southeast Asia, where there has been clinical resistance to [artemisinin],” says Haldar.
She says the situation in Southeast Asia is different because malaria rates are nowhere near as high as in Africa, “and [researchers] understand Southeast Asian parasites – their genetics and their drug resistance profiles – probably a lot better than we do the African parasites.”
Still, there are lessons to be learned from Southeast Asia, including careful monitoring to track how widespread the resistance is and whether there are new mutations. Namazzi says it’s also important to make sure patients — with both uncomplicated malaria and severe malaria — stay on their full dose of medication so as not to breed more resistance.
“Another lesson is that as soon as you’re aware of the problem, you should start thinking of a solution,” says John.
Scientists in Africa and Southeast Asia are studying whether prescribing an additional — third — malaria medication might combat the partial resistance. In addition to the medication options that already exist, Haldar says the study shows “a greater need for new treatment.” But, she says, “the development of a new drug is a very long process” and no new medication is ready to take the place of artemisinin.
Experts say one thing is giving them hope: In the past few years, malaria vaccines have become available.
“All of us in the field feel like it’s a race here — that we need to beat malaria down before there’s widespread drug resistance,” says John.
Sudan’s biggest refugee camp was already struck with famine. Now it’s being shelled
The siege, blamed on the Rapid Support Forces, has sparked a new humanitarian catastrophe and marks an alarming turning point in the Darfur region, already overrun by violence.
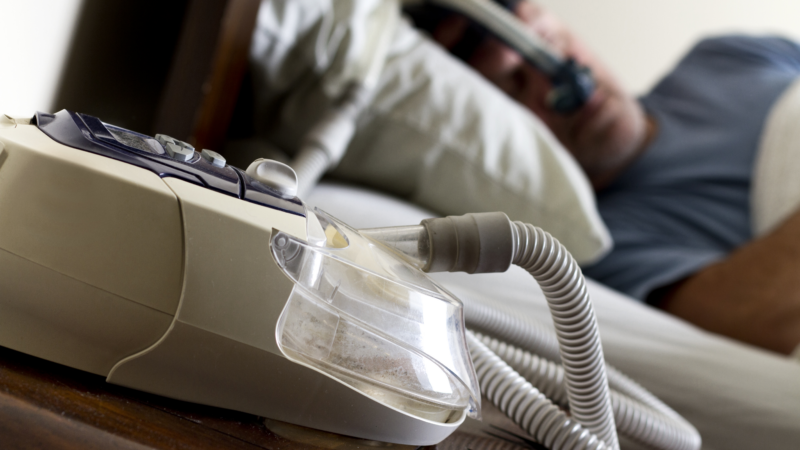
FDA approves weight loss drug Zepbound to treat obstructive sleep apnea
The FDA said studies have shown that by aiding weight loss, Zepbound improves sleep apnea symptoms in some patients.
Netflix is dreaming of a glitch-free Christmas with 2 major NFL games set
It comes weeks after Netflix's attempt to broadcast live boxing between Jake Paul and Mike Tyson was rife with technical glitches.
Opinion: The Pope wants priests to lighten up
A reflection on the comedy stylings of Pope Francis, who is telling priests to lighten up and not be so dour.
The FDA restricts a psychoactive mushroom used in some edibles
The Food and Drug Administration has told food manufacturers the psychoactive mushroom Amanita muscaria isn't authorized for food, including edibles, because it doesn't meet safety standards.
The jury’s in: You won’t miss anything watching this movie from the couch
There's been a bit of consternation flying around about the fact that the theatrical release of Juror #2, directed by Clint Eastwood, was very muted. But this movie is perfect to watch at home.