Physician Suicide
Years of school, long hours and intense pressure – all are part of the deal for young medical students. And once they begin practicing medicine, the amount of mental and physical stress does not subside. Suicide is not an occupational hazard that’s usually discussed in the medical field, but maybe it should be, says Dr. Eva Schernhammer. She teaches at Harvard’s School of Public Health and says a personal tragedy early in her career inspired her decade-long interest in the topic.
“I was still a fellow and I was confronted with a series of suicides that occurred at my hospital. The first of which was actually a very close colleague of mine, a very young resident who was overwhelmed by the work load at the oncology department.”
In 2005, Schernhammer and fellow Harvard scientist Graham Colditz released the largest report of its kind, analyzing 25 other studies of North American and European physicians and suicide rates.
“In this combined analysis we found that there was a higher suicide rate which was statistically significant both for men and women but strikingly higher for the women in those studies.”
They found that male doctors take their own lives at a rate 41% higher than the general public. Female physicians kill themselves at more than twice the rate. Those numbers don’t surprise Dr. Sandra Gomez, a former neurologist at the University of Alabama at Birmingham. She says two colleagues have committed suicide during her 20-year career.
“It’s always been in the back of my mind, how come in such a small circle, where 15 or 20 years ago when I trained, there weren’t so many women in this field and I know two who committed suicide, what’s going on?”
Gomez believes gender bias may be partly to blame. She says women physicians face a lot more pressure than their male counterparts, starting at home.
“When you are a physician, when you are a young woman dealing with marriage, with kids and you know that if you make a mistake, if you prescribe one more milligram of whatever, that patient can die. There is no way you can go home and disconnect. When you get home, you are it. The woman of the marriage is the person that has to deal with everything that goes around in the house. I’m not talking about washing dishes or putting the clothes in the washer and dryer. It’s just everything – we have to move, I have to find an apartment, we need a babysitter, I have to find a babysitter.”
“Oh it’s definitely an issue.”
Dr. Kathe Nelson is Senior Associate Dean for faculty development at UAB. She too has known colleagues that have committed suicide. Her department now has an open dialogue about the stress level that doctors face.
“We have meetings about how to quote “do it all”. As traditional as it sounds, even though more and more men are taking part in child rearing and activities, it seems to fall more on the Mother.”
At a time when more women than ever are entering medical school, it’s an issue that many physicians feel needs to be addressed. According to the Association of American Medical Colleges, women made up the majority of medical school applicants for the first time ever in 2003-2004. Years ago when Birmingham pediatrician Elizabeth Hodges was a medical student the pressure on female students was intense.
“When I was first in medical school in 1978 there were only half a dozen women in the class. One of the women dropped out after a few weeks, the men in the class and the professors were frankly angry, and expressed to us their frustration that she had taken a man’s place and she didn’t go ahead and proceed. That put a lot of pressure on the others of us who did stick it out. Those sorts of attitudes are difficult.”
Even today women doctors say some of those gender biases exist. Anne Wenglarski is an emergency medicine resident who’s been at UAB for a year and a half. This is her second residency. Her first was in orthopedic surgery at another medical school out of state.
“I had thought that I’d always wanted to be in orthopedics and I got there and the residency was not at all what I expected. I felt I was in an unsupportive environment.”
There were only two other women in the program. She was aware of that going in but by the time she arrived, the other female medical student had already resigned and left. Wenglarski acknowledges that one of the reasons she is enjoying her second residency more is the camaraderie among the women.
“There’s more women in the program. My mentor is a female attending. It’s just a different environment altogether, and quite honestly, I don’t think that guys get it as far as things that women feel when they’re getting stressed out in residency. It’s always nice to have someone to relate to and if you don’t have that and if you’re very isolated like how I felt in my other residency, it tends to lead to a very poor outcome.”
Recently, the American Foundation for Suicide Prevention co-sponsored a summit on physician depression and suicide. They talked about the barriers to treatment for depression including lack of time, concerns about confidentiality & stigma, costs of services, and fear of documentation and unwanted intervention. It can be particularly tough for medical professionals to seek help because they worry colleagues will find out. Also – there’s the issue of easy access to medications that could be used in a suicide attempt.
The American Medical Association suggests there needs to be more education among medical professionals and students about recognizing and treating mental disorders and restricted access to lethal drugs. Harvard’s Eva Schernhammer says better social and family support systems are also crucial.
“Each physician who is listening right now should step back for a moment and think about their colleagues, whether there is anyone who they think might be in need of someone to speak with. I would encourage everyone to look after each other because that is the most immediate thing that we could do as physicians.”
Many hospitals do offer employee counseling – but it varies by facility and it’s rarely mandatory.
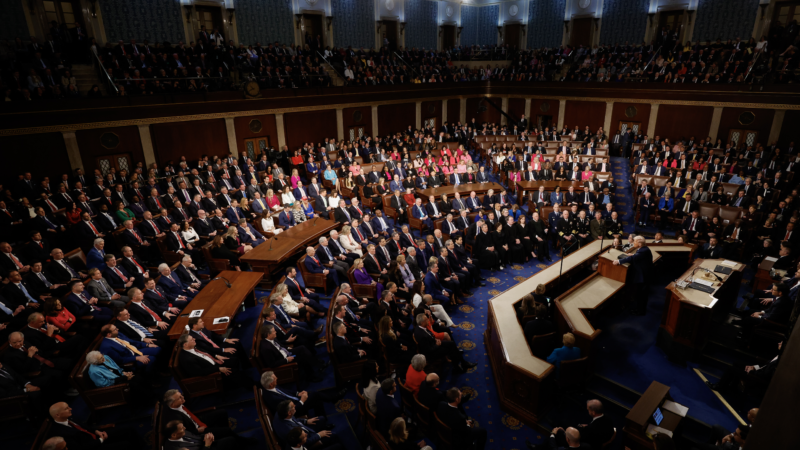
President Trump set to deliver first State of the Union address of his second term
Facing low approval ratings and ahead of midterm elections in November, President Trump delivers the first State of the Union address of his second term as president Tuesday night.
U.S. House rejects aviation safety bill after Pentagon abruptly withdraws support
The House of Representatives narrowly rejected a bipartisan aviation safety bill that was spurred by the deadly midair collision near Washington, D.C. after the Pentagon abruptly withdrew its support.
China and the US alter foreign aid strategies
China's foreign aid strategy has shifted in the last few decades and now its model may be the one the US is adopting as China moves away from it.
Flavor Flav is among women’s hockey team fans outraged by presidential snub
The rapper, who also serves as the official "hype man" for multiple U.S. Olympic teams, invited the female hockey players to Las Vegas for a "real celebration."
Flavor Flav is among women’s hockey team fans outraged by presidential snub
The rapper, who also serves as the official "hype man" for multiple U.S. Olympic teams, invited the female hockey players to Las Vegas for a "real celebration."
Flavor Flav is among women’s hockey team fans outraged by presidential snub
The rapper, who also serves as the official "hype man" for multiple U.S. Olympic teams, invited the female hockey players to Las Vegas for a "real celebration."