Home Mental Health Care
It’s three in the afternoon, and Sandi Partain, is visiting the home of Myra Courtney and her husband in Pell City. Partain is a psychiatric nurse with Alacare Home Health and Hospice, and the Courtney’s are just one of her regular clients. Mrs. Courtney is in her mid to late sixties and is the epitome of Southern grace and charm. When she talks about her parents, she measures her words carefully in a quiet voice, as she lovingly shows their last portrait together before he died.
“My father had Alzheimer’s and my mother has dementia. My father has passed away since then, back in May, and my mother is still with us under our care.”
After a few minutes of small talk, Partain visits Courtney’s 93-year-old mother, who’s resting in her bedroom. Partain engages her in conversation, and gently asks her simple questions, trying to get a read on whether her dementia has worsened. Partain then visits with Courtney and her husband, asking how they are coping, and if they have any questions for her.
Partain is one of a growing number of psychiatric nurses breathing life into the old term “house-call.” According to Dr. Richard Powers, medical director of the Alabama Department of Mental Health and Retardation, 10 percent of people over the age of 65, and almost half of people over the age of 85 suffer from some sort of intellectual impairment. Most often it’s dementia. Depression is common as well.
“So consequently, for a variety of reasons, as an aging society, we’re going to need more and more help being able to stay at home.”
But finding the patients who can benefit from in-home care can be the elusive piece of this home health care puzzle. Again, psychiatric nurse Sandy Partain.
“Sometimes we get referrals from patients who have been hospitalized in a psychiatric unit, and we will get the referral through the discharge planner at the hospital, and go out and admit them after that. Sometimes they have just seen the physician in the office and the physician feels like they would be appropriate for home care.”
Sometimes a family will call Alacare directly. That usually signals they’ve exhausted the resources with their family doc and are at the end of their rope.
“Each patient is an individual and has a unique situation.”
Dr. Tera Bryant, Corporate Medical Director for Alacare.
“And, many times you have a family member calling the office repeatedly, and you understand their stress level is very high regarding the issues and the patient may not be making it to the office, and those are red flags that are telling the physician I need some help out in the community.”
When visiting the home, the nurse first develops a relationship with the patient and family. He or she then teaches them about the patient’s particular diagnosis, what’s occurring and why it’s happening. The nurse also instructs everyone when it’s time to call for help. For Myra Courtney, the help has been invaluable.
“They really, really helped me understand the illness. And, it helped me understand how to relate to them better, how to understand, especially the dementia. Well, the Alzheimer’s too, actually.”
Another benefit of these “house calls” is observing the patient at home. Dr. Bryant says often times, a patient brings their “A” game to the doctor’s office, and families are on their best behavior.
“We all want to look good and feel good and demonstrate that to our doctor. And, the nurse going into the home really gives a much better picture of what’s going on, on a day-to-day basis. And, I love the nurses to go out and the patient to do well, but the best thing that can happen is that the nurse goes out and when there’s a day that’s in crisis, to help the family, as well as the patient to understand why that’s occurring.”
“The problem with dementia, in addition to making folks forgetful, it also produces personality changes, and new behavioral or psychiatric problems.”
Again, Dr. Richard Powers of the Alabama Department of Mental Health and Retardation
“The simple stuff are things like competitive questions that can be dealt with. However, other stuff like trying to escape from the house. Trying to steal car keys and drive at risk to other people.”
“They can be a life saver to the caregiver. Caregivers, most long term for older people is provided by family members…it’s usually a woman between the ages of 45 and 65. It could be a spouse or daughter, often times, they’re just getting their kids out of the house, and they’re getting to the point, kind of established in the job, and their thinking they’re going to enjoy life. Before you know it, they’ve having to take care of mom or dad and that can be very distressing.”
But what about the stress on the psychiatric nurses who are bringing so much comfort and support to these households? Sandi Partain says it can be stressful.
“But as psychiatric nurses, we know, we teach other people how to cope with things. So, hopefully we use those same coping techniques ourselves. But usually, we are able to improve their situation to the point that they feel so much relief, that we actually feel good about what’s happening. . .and at least you go home at night knowing that you made a little bit of difference, and everybody feels a little better.”
As the general population ages and our bodies outlast our minds, thousands of families will find themselves in the unfamiliar, terrifying terrain of caring for a loved one with mental illness. And, as that trend continues to grow, the experienced psychiatric nurse could become more vital than ever before, for both the patients and their caregivers.
Mideast clashes breach Olympic truce as athletes gather for Winter Paralympic Games
Fighting intensified in the Middle East during the Olympic truce, in effect through March 15. Flights are being disrupted as athletes and families converge on Italy for the Winter Paralympics.
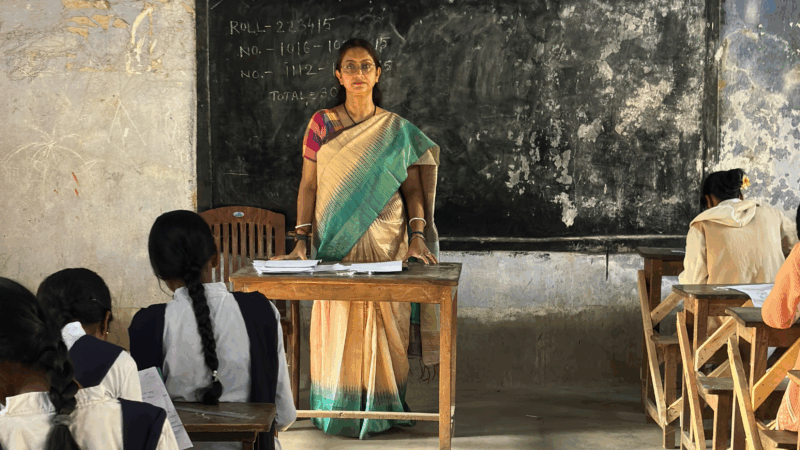
A U.S. scholarship thrills a teacher in India. Then came the soul-crushing questions
She was thrilled to become the first teacher from a government-sponsored school in India to get a Fulbright exchange award to learn from U.S. schools. People asked two questions that clouded her joy.
U.S.-Israeli strikes in Iran continue into 2nd day, as the region faces turmoil
Israel said on Sunday it had launched more attacks on Iran, while the Iranian government continued strikes on Israel and on U.S. targets in Gulf states, Iraq and Jordan.
Trump warns Iran not to retaliate after Ayatollah Ali Khamenei is killed
The Iranian government has announced 40 days of mourning. The country's supreme leader was killed following an attack launched by the U.S. and Israel on Saturday against Iran.
Iran fires missiles at Israel and Gulf states after U.S.-Israeli strike kills Khamenei
Iran fired missiles at targets in Israel and Gulf Arab states Sunday after vowing massive retaliation for the killing of Supreme Leader Ayatollah Ali Khamenei by the United States and Israel.
Iran’s Ayatollah Ali Khamenei is killed in Israeli strike, ending 36-year iron rule
Khamenei, the Islamic Republic's second supreme leader, has been killed. He had held power since 1989, guiding Iran through difficult times — and overseeing the violent suppression of dissent.