‘It’s A Reality For Us.’ ICU Nurse Shares The Impact Of COVID-19
Despite recent record-breaking numbers of new coronavirus infections and hospitalizations in Alabama, health experts say many people are not taking the virus seriously.
“A lot of people don’t know anyone with COVID,” UAB infectious disease specialist Dr. Jeanne Marrazzo said during a recent press conference. “A lot of people have never been in an intensive care unit. A lot of people have never seen a patient on a ventilator or been on a ventilator. I guarantee you if you took care of patients on ventilators or spent some time in the ICU taking care of COVID patients, I think you would wear a mask.”
So what is it like inside an intensive care unit right now?
Kelsey Jacks, a registered nurse in the Medical ICU at UAB Hospital, has been taking care of critically ill patients diagnosed with COVID-19 for the past several months. She shared this audio diary that she recorded during a shift last week.
“Your Day Can Look Like Anything”
I just got to work and have parked in the parking deck. It is 6:17 in the morning and I am just sitting in my car and am in denial about waking up and going into work. No, really I’m just I’m buying a few more minutes of peace and quiet and getting to sit down before I go in and start the day.
I don’t know what my assignment’s going to be like today, so I’m kind of anxious about that. Your day can look like anything. Sometimes you can walk in and have stable patients, you know, they’re still on life support, but nothing big is happening with them at that moment. And then there’s a lot of these patients who are in acute respiratory failure, and we have to do this, I guess it’s a procedure. It’s this therapy called manual proning, and it’s where the nurses and the respiratory therapists will physically turn a patient and lay them on their stomach. And that essentially helps the lungs to recruit more oxygen and perfuse properly and just heal from what this virus has done to their lungs. But all of these people are on the ventilator and sedated, so they’re just flaccid and you’re having to pick up their whole body weight on your own. So it’s just, it’s physically exhausting.
So my day so far, both of my patients that I’m taking care of, I just have developed a kind of just a bond or an attachment to. One of the patients is very sick. They’re on multiple I.V. drips. She’s on her stomach and just very unstable. Every time I try to leave the room, something decompensates and I have to put on all the gear and go back in, so I just haven’t been able to get away from that room this morning.
The Hardest Part
It’s been overwhelming at times. I mean, all of us nurses and [respiratory therapists] and nurse practitioners and doctors will talk about how we’ve all had moments where we just, we just break down from the overwhelming stress of seeing people with this illness and then wondering if you have it yourself and knowing how bad it can get.
I think the hardest part has been having to watch people die alone. I’m so sick of that. You know, these patients, they can’t have their visitors come and see them because it’s too much of a risk. Sometimes family can come and say bye, but only for about 20 minutes because when you take someone off the ventilator, that’s one of the most dangerous times that you can get coronavirus. So families will come and say bye to a patient before they are taken off the ventilator. And then when they leave is when we actually withdraw the life support and begin the end-of-life process. And it takes a piece of you every time that you do it because it’s just so sad. And I can’t tell you the dozens and dozens of faces of patients and family members I remember just over the past few months. And it just stays with you. But those are also the moments when I feel most proud to be a nurse or when I am most proud of my coworkers and my work family.
There was one instance wherein a nurse and a nurse practitioner put on all the protective gear and just went and sat in a room with the patient and just held her hand for hours as she passed and they gave her medicines to make her comfortable and played her favorite music and read to her. And it was just, it was just beautiful and tragic. And those are the stories that I wish we’re told more often. And those are the things that I wish the public knew. But that’s the most difficult thing for me. And I hope that by hearing about this for people who aren’t in health care, you kind of understand more of our passion as health care workers for the social distancing movement and wearing masks. Because when we say those things, it’s because we’ve had to literally be in the room when people die from it. It’s a reality for us and it is a reality.
This audio diary has been edited for length and clarity.
Why farmers in California are backing a giant solar farm
Many farmers have had to fallow land as a state law comes into effect limiting their access to water. There's now a push to develop some of that land… into solar farms.
Every business wants your review. What’s with the feedback frenzy?
Customers want to read reviews and businesses need reviews to attract customers. But the constant demand for reviews could be creating a feedback backlash, experts say.
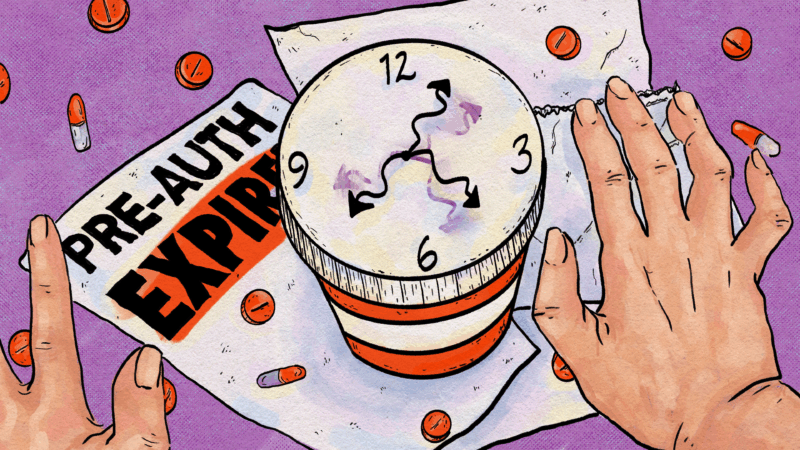
Can’t get a prescription renewed? Here’s how to cope with prior authorizations
These health care hurdles can stand in the way of getting treatment your doctor says you need. Here's what to know about how to deal with them.
‘Get back to integrity’: Oklahoma’s Kevin Stitt on Republicans after Trump
NPR's Steve Inskeep asks Oklahoma Gov. Kevin Stitt about his spat with President Trump, immigration and the future of the Republican Party.
Civil rights leaders say the racial progress Jesse Jackson fought for is under threat
Activists say racial progress won by the Rev. Jesse Jackson is under threat, as a new generation of leaders works to preserve hard-fought civil rights gains.
Tariffs cost American shoppers. They’re unlikely to get that money back
After the Supreme Court declared the emergency tariffs illegal, the refund process will be messy and will go to businesses first.