You Know Delta, But Have You Met Mu And The Rest Of The Relatives?
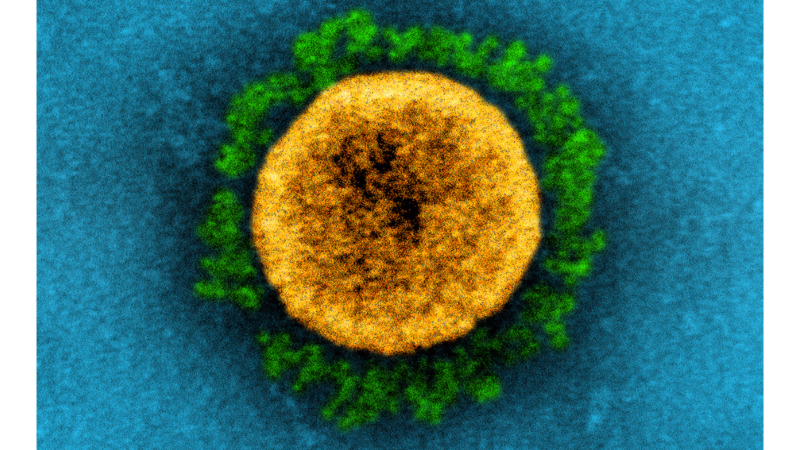
Transmission electron micrograph of a SARS-CoV-2 virus particle. The prominent green projections seen on the outside of the yellow virus particle are spike proteins. This fringe of proteins enables the virus to attach to and infect host cells and then replicate.
Viruses mutate.
Researchers say there always will be new variant strains of the COVID-19 virus, although all the strains won’t be as deadly as delta.
The delta strain has made COVID more deadly for the unvaccinated. It is responsible for 90% of the 40 million COVID cases in the U.S and the deaths of 648,000 people, according to the Centers for Disease Control and Prevention. It also spreads much faster and may cause more severe cases than other variants, according to the CDC.
But the delta strain is not alone. There are many variants being studied by researchers and scientists.
Last Friday, the World Health Organization added the mu strain to its list of COVID variants of interest. It joins eta, iota, kappa and lambda on the list.
The mu variant does not yet account for a substantial portion of infections in the U.S. There are 2,000 mu cases in the U.S. The strain has been detected in 39 countries and in minute numbers in 45 states, including Alabama, but it is more prevalent in Texas, Florida, California and New York.
“We are keeping a close eye on mu,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases and chief medical adviser to President Biden.
The mu strain became a variant of interest after increases in the number of cases in South America, particularly Columbia, Peru, Ecuador and Chile.
The strain needs further study to confirm whether it will be more contagious, more deadly or more resistant to current vaccines and treatments, according to the WHO.
“It is always difficult to predict when rising variants will become a problem,” said Kevin Harrod, UAB professor and researcher of infectious and respiratory diseases.
With the delta variant, the rapid rise in cases and rapid replacement of the alpha strain clearly indicated that this variant would be very prevalent, Harrod said.
Mu has the potential to be problematic because the variant has a constellation of mutations that have “potential properties of immune escape,” according to World Health Organization. That means that natural immunity, vaccines or monoclonal antibodies therapy may not work as well.
U.S. health officials stress that mu is not an immediate threat to this country.
“We are paying attention to it, we take everything like that seriously, but we don’t consider it an immediate threat right now,” Fauci said last Thursday.
Variants of Interest
The CDC classifies variants “of interest” if they show specific genetic markers that have been associated with changes to receptor binding, reduced neutralization by antibodies generated against previous infection or vaccination, reduced efficacy of treatments, potential diagnostic impact, or predicted increase in transmissibility or severity.
“We will probably have … what we call a variant of interest identified every few weeks,” said Dr. Allison Arwady, commissioner for the Chicago Department of Health.
She explained that it means there have been a number of genetic mutations emerging, and scientists around the world are on the lookout for new ones. This information gets updated in a database that is shared internationally.
COVID variant names sound like sorority row because the names come from the Greek alphabet. The CDC added mu to its list of strains “of interest,” joining alpha, beta, gamma and delta.
Details of the list, other than mu include:
Alpha B.1.1.7
The variant was first identified in the United Kingdom and quickly spread in the U.S. before the delta variant took hold.
Alpha spreads fast, and people get sicker or die, according to the CDC.
Vaccines in the U.S. work against this variant, although some breakthrough cases have been reported, the vaccines continue to prove effective against severe illness, hospitalization and death, the CDC says.
“From April through the summer, delta almost completely replaced the alpha variant in the U.S.,” said UAB’s Harrod. “This is quite extraordinary given the magnitude of infection that existed prior.”
Harrod explained that variants are typically discovered through testing. As an example, the alpha variant was discovered in the United Kingdom when one of three tests in the PCR assay started showing negative results when the other two were positive for the same individual. The mutation occurred at the site in the viral genome where the PCR would detect the virus.
PCR stands for a polymerase chain reaction test. It detects genetic material from a specific organism, such as a virus.
Beta B.1.315
It was first identified in South Africa, and it may spread faster than other variants. But current CDC data has shown no sign that the variant causes “more severe illness, hospitalizations and deaths.” U.S. vaccines work, but certain monoclonal antibodies treatments are less effective.
Gamma P.1
It was first identified in Japan and Brazil. It spreads faster than some other variants, but there are no signs that it causes more severe illness or death. Vaccines work. Some monoclonal therapies do not.
Delta B.1.617.2
The CDC says the variant’s speed and transmissibility cause more severe cases than other variants.
Delta’s fast spread makes it able to “pick off the more vulnerable more efficiently than other variants,” said Dr. Mike Ryan, director of WHO’s health emergencies program. The variant also “poses a particular threat to young people,” said White House coronavirus response coordinator Jeff Zients.
Fully vaccinated people who become infected can spread this virus. Monoclonal antibody therapy can make it less severe.
Each variant has a certain set of mutations. Delta has a set of mutations that make it excellent at infecting people, said Dr. F. Perry Wilson, a Yale Medicine physician and researcher at Yale School of Medicine.
“That is why it is rapidly taking over.”
Delta Plus AY.1
There is no evidence that this variant will be more of a problem or more of an issue than the original delta variant.
“Right now, there is no reason to believe that delta plus is going to pose any more challenge above and beyond delta, but obviously we need more data,” said Dr. Amesh Adalja, senior scholar at the Johns Hopkins University Center for Health Security.
It is more contagious but responsible for less than 1% of COVID cases.
“Delta plus is a media term,” Harrod said. “I don’t really know what that means, but further evolution of the Delta strain is likely given the amount of virus circulating in the community, the large numbers of unvaccinated individuals, and the beginning of in-person learning in schools with little use of protective measures.”
Eta
Eta is being monitored by WHO but has not been identified in the U.S.
Iota and Lambda C.37
Iota, which first was identified in New York, and lambda are listed as viruses of concern by the WHO, but not the CDC.
Iota has been detected in 29 countries, and it may spread more quickly than milder versions of the virus. It has been spreading rapidly in South America, promoting more investigation of this variant.
A variant is placed on the “of concern” list once researchers see it clearly has an impact, according to the CDC.
When that happens, the CDC and others want to investigate why more people are being infected with variants, sometimes because it is more transmissible or infectious, like the Delta variant is.
Sometimes it may be because the virus can escape the immunity induced by the vaccine. This latter possibility has not happened on any significant scale yet.
The third classification is a variant “of high consequences” once evidence is seen that preventative measures or countermeasures have significantly reduced effectiveness relative to previously circulating variants. None have been identified at this time.
UAB’s Harrod disputes whether delta responds to some of the therapeutic antibodies that are used in patient treatment.
“I have yet to see any data that all therapeutic antibodies are less efficacious to delta infections. So far, at least one of the four or five therapeutic antibodies in use is very effective against all variants that are circulating,” he said.
With more variants circulating, it will be important to have accurate information on the strain infecting an individual, so the most effective therapeutic antibody can be given to the patient, he added.
“I doubt this is done in most clinical settings though. Outer-lying community hospitals will only have the budget for maybe one or two therapeutic antibodies and probably won’t have the testing in place to fully sequence the virus or even detect the specific strain.
“It is really these types of scenarios that make the mutating viruses more concerning,” Harrod said.
Pentagon puts Scouts ‘on notice’ over DEI and girl-centered policies
After threatening to sever ties with the organization formerly known as the Boy Scouts, Defense Secretary Hegseth announced a 6-month reprieve
President Trump bans Anthropic from use in government systems
Trump called the AI lab a "RADICAL LEFT, WOKE COMPANY" in a social media post. The Pentagon also ordered all military contractors to stop doing business with Anthropic.
HUD proposes time limits and work requirements for rental aid
The rule would allow housing agencies and landlords to impose such requirements "to encourage self-sufficiency." Critics say most who can work already do, but their wages are low.
Paramount and Warner Bros’ deal is about merging studios, and a whole lot more
The nearly $111 billion marriage would unite Paramount and Warner film studios, streamers and television properties — including CNN — under the control of the wealthy Ellison family.
A new film follows Paul McCartney’s 2nd act after The Beatles’ breakup
While previous documentaries captured the frenzy of Beatlemania, Man on the Run focuses on McCartney in the years between the band's breakup and John Lennon's death.
An aspiring dancer. A wealthy benefactor. And ‘Dreams’ turned to nightmare
A new psychological drama from Mexican filmmaker Michel Franco centers on the torrid affair between a wealthy San Francisco philanthropist and an undocumented immigrant who aspires to be a dancer.