Its Future In Limbo, Limiting Telehealth In The Gulf South Could Be Troublesome For Rural Areas
Dr. Eric Wallace, medical director of the University of Alabama at Birmingham Telemedicine, is visible on a UAB eMedicine screen in 2019.
For patients living in rural Alabama, a trip to a specialist physician could mean driving for over an hour.
That is the case for Patrick Stults, who drives south from Haleyville to Birmingham every month for dialysis treatments and bloodwork. But in between those trips, he uses telehealth — a service that has grown exponentially in usage during the COVID-19 pandemic.
“I like it because you can see the doctor face to face, and if you have any problems you can talk to them,” Stults said.
Telehealth became a necessity while many people were sheltering at home because of state lockdown laws. The nonprofit group FAIR health, which tracks billions of private hospital bills, estimates a nearly 3,000% increase in the number of telehealth claims between Dec. 2019 and December 2020.
And while telehealth is likely to stay a part of Stults’ and many other patients’ lives in the Gulf South, laws that have made it more available could go away post-pandemic. That could leave the region’s more rural areas hurting the most due to access barriers and disparities.
Expanding Coverage For Telehealth
Before last year, it was difficult for hospitals and clinics to bill insurance for a telehealth visit. Typically, doctors could not be reimbursed by insurance for phone call visits the same way as an in-person one, or there was no reimbursement at all.
But during the COVID-19 pandemic, many policies changed to allow those charges, and people could be taken care of while they were staying at home.
Some states, like Mississippi, even broadened what types of telehealth could be covered by Medicaid.
“You probably have folks who maybe weren’t seeking out mental health services before, but are now looking for it,” said Mei Kwong, the executive director at the Center for Connected Health Policy.
While telehealth utilization has dropped from the highs it saw at the beginning of the pandemic, its usage is still higher than it was pre-pandemic, Kwong said, thanks to the more flexible policies put in place.
Despite Benefits, Disparities Need To Be Addressed
Telehealth was helpful for Stults, who has had a lot of health emergencies, long before the pandemic started. The 47-year-old uses telehealth as a way to give himself peace of mind in between his monthly in-person visits.
“All we do is just answer questions like if I’m doing okay, or if I have swelling in my legs or if my sight is okay,” Stults said.
Stults’ doctor, nephrologist Eric Wallace from the University of Alabama at Birmingham, started a telehealth program for his rural patients in 2015. The school worked with the Alabama Department of Health to set up remote video-conferencing centers at rural health departments in different counties across the state.
Stults is familiar with technology and said it was not hard for him to go to these county sites, but even when telehealth is offered, that does not mean disparities automatically go away.
Wallace says telehealth — particularly the kind that is delivered in a patient’s home — is necessary and helpful for some patients who want to receive some of their medical care that way. But it’s not always convenient, and other patients have faced a lot of hurdles.
“Number one is, ‘I don’t have the money for a phone, or I don’t have a phone,’” Wallace said.” Number two is, ‘I don’t have internet, or I don’t have the money to pay for it.’ This is probably the most common.
“Number three is, ‘I have a phone. I have the money to buy internet. But I don’t know how to use it.’”
According to 2018 Census data, 1 in 4 rural residents across the Gulf South lack a subscription to the internet. Across the U.S., that average is 1 in 5.
Wallace says some studies show patients who would skip out on seeing the doctor altogether could be more likely to get medical attention if telemedicine is an option. Others might want to go to the doctor and just need help with transportation or getting insurance. But telehealth cannot and should not be used for all types of care, Wallace said.
“For dialysis care, patients have to come in once a month. They have to get labs. And so my telehealth was always about giving patients choice,” he said. “For me, telehealth doesn’t necessarily mean I’m going to do a better job. It’s about how I want my patients to have the best quality of life.”
A Lifeline For Rural Communities
The federal government also recognizes there are barriers to telehealth access. The U.S. Department of Agriculture announced in February that it is investing over $40 million in telemedicine and distance learning infrastructure in rural areas through a series of grants. From those grants, more than $5 million is going toward telemedicine projects in Mississippi and Alabama.
However, the pandemic-related policies that made telehealth more available to patients could expire at the end of the health emergency. And, the Gulf South might feel it the most.
The region is more rural than the rest of the country, with more people spread out far away from health centers. Centers for Disease Control and Prevention data show that people in Alabama, Louisiana and Mississippi often deal with high rates of chronic health conditions like hypertension, obesity, and heart failure.
Adding to the region’s problems is a below-average number of primary care physicians available. In the U.S., there are about 90 primary care physicians for every 100,000 people. Each Gulf South state, however, is well below that median — Mississippi only has 66 physicians, Alabama only has 77 and Louisiana only has 84, according to a 2019 report from the Association of American Medical Colleges.
“We have one of the lowest numbers of primary care physicians in the state of Mississippi,” said Dr. Saurabh Chandra, chief telehealth officer at the University of Mississippi Medical Center. “Then you look at how spread out the rural areas are … it means less access to primary care.”
Hospitals like the UMMC and the University of Alabama at Birmingham have invested in telehealth long before the pandemic. Chandra says the center recognized the benefits of telehealth over a decade ago to try to reduce the physician-to-patient gap.
Chandra says he believes those flexible insurance policies from the COVID-19 pandemic have been helpful and ought to stay in place.
He acknowledges there is a risk of creating a gap between “the haves and the have-nots” when it comes to patients who are not as tech-savvy or cannot afford the technology. But he says it’s important to invest in telehealth because that is the only way to prove that closing that gap is important.
“That’s how private companies or the federal government will see the value [of telehealth] and create the infrastructure so that people who are being left behind can get access to it,” Chandra said.
This story was produced by the Gulf States Newsroom, a collaboration between Mississippi Public Broadcasting, WBHM in Birmingham, Alabama, WWNO in New Orleans and NPR.
Editor’s Note: UAB holds WBHM’s broadcast license, but our news and business departments operate independently.
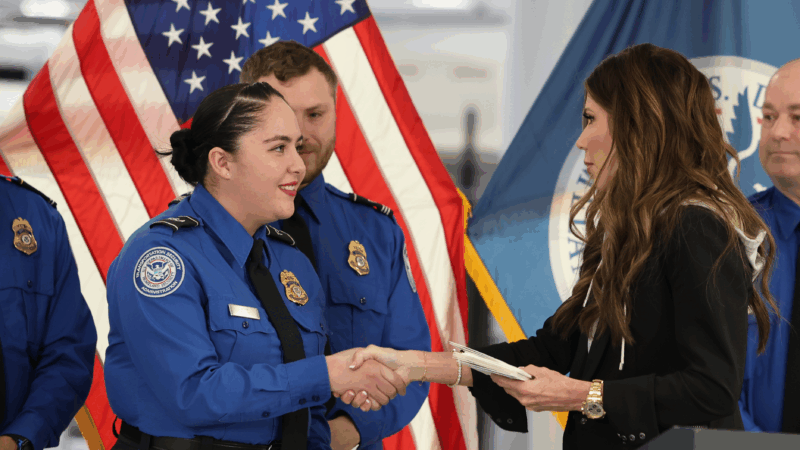
Homeland Security suspends TSA PreCheck and Global Entry airport security programs
The U.S. Department of Homeland Security is suspending the TSA PreCheck and Global Entry airport security programs as a partial government shutdown continues.
FCC calls for more ‘patriotic, pro-America’ programming in runup to 250th anniversary
The "Pledge America Campaign" urges broadcasters to focus on programming that highlights "the historic accomplishments of this great nation from our founding through the Trump Administration today."
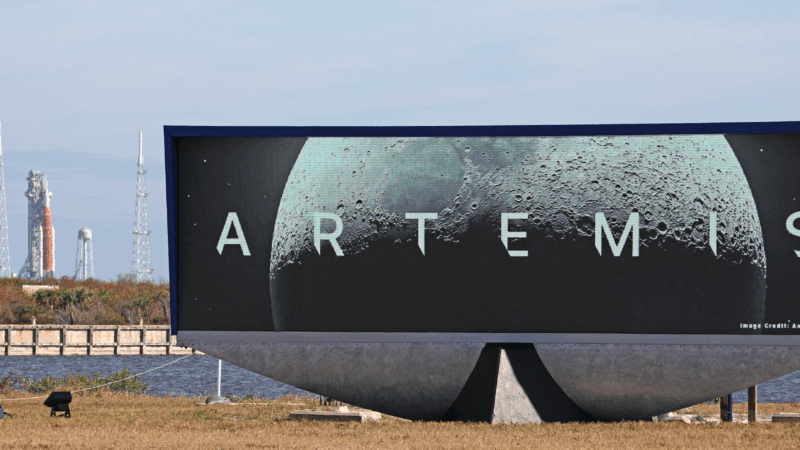
NASA’s Artemis II lunar mission may not launch in March after all
NASA says an "interrupted flow" of helium to the rocket system could require a rollback to the Vehicle Assembly Building. If it happens, NASA says the launch to the moon would be delayed until April.
Mississippi health system shuts down clinics statewide after ransomware attack
The attack was launched on Thursday and prompted hospital officials to close all of its 35 clinics across the state.
Blizzard conditions and high winds forecast for NYC, East coast
The winter storm is expected to bring blizzard conditions and possibly up to 2 feet of snow in New York City.
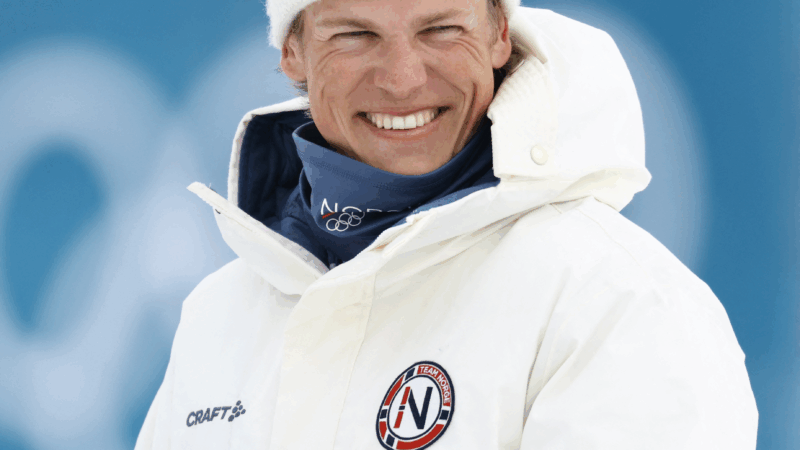
Norway’s Johannes Klæbo is new Winter Olympics king
Johannes Klaebo won all six cross-country skiing events at this year's Winter Olympics, the surpassing Eric Heiden's five golds in 1980.