Why certain medications can increase your risk in the heat
For the millions of Americans who take medications for common issues like heart disease or high blood pressure, a heatwave like the one causing sweltering conditions across the Central and Southeastern U.S. this week poses extra risk.
That’s because some medications can change how people’s bodies naturally manage heat, says David Eisenman, a physician and researcher at the University of California, Los Angeles, potentially making people more susceptible to overheating.
Eisenman stresses that patients should still take their medications. But he urges them to take the risks from heat seriously and develop a plan to keep cool — by taking steps like cooling their homes with air conditioning or fans, drinking water and staying out of the hot sun.
Why do some medications affect heat tolerance?
The consequences of overheating can be dramatic: an overstrained heart, kidney issues, brain damage and even death are possible when internal temperatures climb too high for too long.
“I think of core temperature as your body’s internal temperature like a car engine,” says Eisenman. A car, like a body, needs to keep its engine at a reasonable temperature.
Bodies adjust in many ways. They can calibrate the amount and saltiness of sweat. A mechanism in your brain can trigger a sensation of thirst, prompting you to drink enough water to create enough sweat. The vascular system shunts more blood toward the skin, where it can be cooled by breeze or evaporating sweat.
But some classes of medications — from some beta blockers to diuretics to antidepressants — can affect the way people’s bodies react to, or perceive, heat. ACE inhibitors, commonly prescribed for heart issues, make it harder to realize you’re thirsty, and beta blockers — another heart medication — can decrease sweating, making it harder to cool off.
“When you’re taking these medications and you’re exposed to heat, it’s like asking a car to drive up a mountain in the summer with the air conditioner broken, low on coolant and no warning signals,” Eisenman says. “Overheating becomes much more likely.”
That doesn’t mean you should stop taking your medications during heat waves, Eisenman stresses. It means keeping yourself from getting too hot in the first place. “Making sure people have access to a cool space” should be the priority, he says, whether that’s running an air conditioner at home or finding a local cooling center.
What medications increase heat risk?
The Centers for Disease Control and Prevention catalogs many different medications that could interfere with the body’s heat management system, based on how different types of drugs work.
- Millions of Americans take ACE inhibitors or ARBs to manage high blood pressure. But they can affect people’s ability to sense thirst, potentially leaving them dehydrated.
- Beta blockers can keep blood from flowing toward the skin, where it can cool, and decrease sweat.
- Diuretics, commonly prescribed for kidney problems, may contribute to dehydration.
- Anticholinergic medications — including some over-the-counter antihistamines, like Benadryl — can reduce sweating.
- Antipsychotics can make it harder for people to sense their own temperature, so they can’t tell when they’re overheating.
Many other drugs, including ADHD medications and some antidepressants, could also influence heat risk.
Older people generally have a harder time managing heat even without added medication risks, says Rutgers University physician and researcher Soko Setaguchi. She led a study focused on Medicare patients — all of whom were older than 65 — that found the chance of ending up in the hospital after summer heat waves was higher for those taking anticholinergics and antipsychotics, along with ACE-inhibitors.
But like Eisenman, she stresses that patients shouldn’t stop taking medications when it’s hot. “The message for now is, there are potential risks,” she says, so patients should strive to “avoid heat, anticipate heat and plan for heat.”
What is still unknown?
The theoretical ways drugs can affect heat tolerance are well-known, but there haven’t been enough systematic analyses looking at how, and at what levels, and for whom drugs affect heat tolerance, says Yorgi Mavros, a heat expert at The University of Sydney. But some messages have begun to emerge.
During the heat dome that descended on the Pacific Northwest in 2021, people who had been prescribed medications, including anti-epileptic drugs, antipsychotics and some beta blockers, were more likely to have died during the extreme heat than people who hadn’t been prescribed those drugs.
Another study looked at the risk of heart attacks during extreme heat events in Germany. The chance of dying went up if patients had used anti-platelet medication and beta-receptor blockers, compared to patients who weren’t on the medications.
Another looked at the effect of different medications on kidney-related hospitalizations in the Atlanta area during the summer months. Patients on antidepressants and patients taking multiple medications at once ended up in the hospital at a higher rate, says lead researcher Zachary McCann, who was at Emory University at the time the study was published.
It’s common that patients will take many medications at once, says McCann. Yet, he says, the combined risks have not been assessed thoroughly — a concern echoed by Eisenman and Mavros.
The urgency to answer some of these questions is growing, says McCann. Climate change intensifies heat, stretches the length of heat waves and drags summers later into the year.
“Summers are going to get hotter. They’re going to get longer,” he says. “We know that heat causes dysregulation of all kinds of organ systems and wreaks havoc on the body in all kinds of different ways.” So, McCann says it’s critical that patients and doctors work together to make plans to protect themselves.
“Prevention is really the best medication when it comes to the management of heat,” he says.
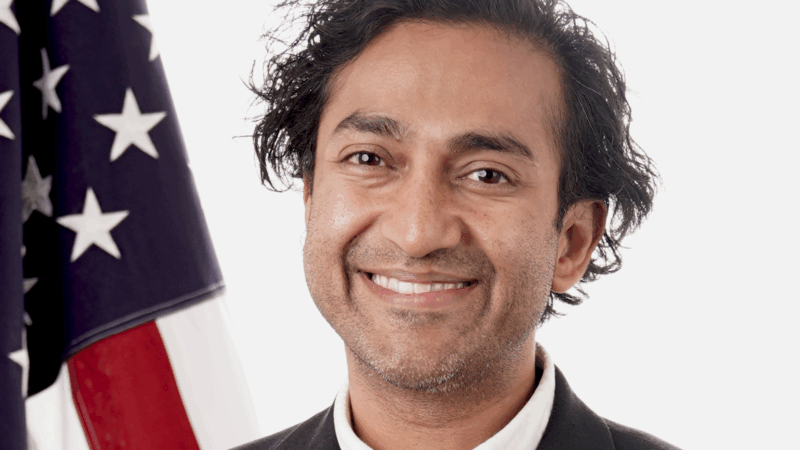
Trump administration’s embattled FDA vaccine chief is leaving for the second time
The FDA's controversial vaccine chief, Dr. Vinay Prasad, is leaving the agency. It's the second time he has abruptly departed following decisions involving the review of vaccinations and specialty drugs.
Family, former presidents and a Hall of Famer give Rev. Jesse Jackson a final sendoff
Several speakers at Jackson's funeral invoked his hallmark catchphrases: "Keep hope alive" and "I am somebody."
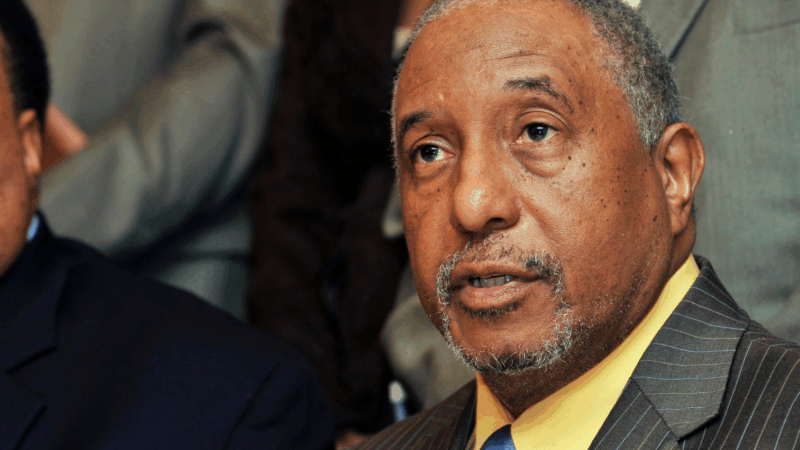
Bernard LaFayette, Selma voting rights organizer, dies at 85
Bernard LaFayette, who died Thursday, laid the foundations of the Selma, Alabama, campaign that culminated in the passage of the Voting Rights Act. He was a Freedom Rider and helped found the Student Nonviolent Coordinating Committee.
Oil surges to its highest price since 2023, and stocks drop after U.S. jobs report
Stocks fell Friday on worries that the economy could become stuck in a worst-case scenario of stagnating growth and high inflation. Oil prices touched their highest levels since 2023 after surging again because of the Iran war.
No lawsuits required: U.S. Customs is working on a system to refund tariffs
U.S. Customs told the trade court it aims for a streamlined process in 45 days to return importers' money without requiring individual lawsuits.
Poll: A majority of Americans opposes U.S. military action in Iran
Most Americans disapprove of President Trump's handling of Iran, and a majority sees Iran as either only a minor threat or no threat at all, an NPR/PBS News/Marist poll finds.