The U.N. utters the word: Dementia
For the first time, a United Nations declaration is pledging to address dementia.
On Thursday, world leaders at the U.N. General Assembly in New York are laying out a new plan for combatting mental health challenges and non-communicable diseases. While their political declaration emphasizes conditions like cardiovascular disease and diabetes, it also mentions neurological conditions like dementia.
“It’s historical for us. It’s a real watershed moment,” says Paola Barbarino, CEO of Alzheimer’s Disease International, the advocacy group with members in 105 countries.
She said the inclusion of dementia is particularly significant for lower-income countries, many of which are still in “denial” about the condition.
Even in high-income countries where dementia gets attention, like the U.S., it has been a struggle to bring about the behavioral changes and medical interventions — such as weight loss and better blood pressure control — that could delay the onset of the condition. And, for many families dealing with dementia, finding adequate care and support is far from easy.
While the World Health Organization did put forward a global action plan on dementia in 2017, which was extended earlier this year, Barbarino says, dementia is often missing or minimized in major policies, frameworks and discussions about non-communicable diseases. For example, WHO’s 2022 report Invisible Numbers: The True Extent of Non-communicable Diseases and What To Do About Them didn’t mention it. And in 2011 the U.N. did mention Alzheimer’s disease in a declaration but did not make specific commitments to address dementia.
WHO emailed this statement to NPR on Thursday: “The 2025 declaration marks a significant milestone by recognizing the global impact of dementia and committing to scale up access to services for the 57 million people living with the condition worldwide.”
NPR caught up with Barbarino — who has spent years as an activist and advocate — while she was in New York for the U.N. General Assembly to talk about the significance of this moment and what comes next. This interview has been edited for length and clarity.
Why does this matter?
Dementia is one of the biggest health and care challenges of our time. And it’s set to grow a lot in prevalence as the population gets older.
Just to give you an idea, last week, Australia declared dementia to be the leading cause of death. It is already among the biggest causes of death in the U.K., in the Netherlands, in Finland — in a lot more countries.
So it’s actually extraordinary that it wasn’t already included [in a U.N. declaration]. But this was not out of spite. It’s simply because the stigma around dementia was so fierce that in the 1980s — when there was a movement for the other non-communicable diseases like cancer, diabetes, respiratory disease — nobody was speaking about dementia.
What did it take for dementia to be included?
It has been probably two years of very serious work. We knew it was a problem beforehand but only recently did we realize that non-communicable disease mortality data [published by the World Health Organization often] focused on people below 70 years of age and not those above 70 years of age. Now, considering people are dying later, we cannot possibly not consider those last 20-some years of [life]. And it’s in those 20 years, it’s most likely that people will develop dementia.
So we spent time collecting the data, doing evidence-based research. We published an article in Nature Review Neurology in January. Dementia is expected to be the third leading cause of death globally in 2040. And people have listened.
What does this declaration mean for countries?
So, for high-income countries, a lot of the risk reduction factors for dementia [like anti-smoking efforts and campaigns to increase physical activity] are the same as those for other major diseases like cancer and cardiovascular disease. So governments can embrace this agenda a lot more solidly.
A lot of low-income countries are still in denial about the fact that dementia is a big problem in their country. That stems from the fact that, in part, they consider themselves young countries, with more young people than old people. They’re just not used to thinking about what’s going to happen to the older population.
Often, when our members [in lower-income countries] ask for their government to have risk reduction campaigns, they are told that dementia is not a big condition in the country. Sadly, that [kind of denial] means people living with dementia are not receiving the care and support that they deserve. Same with caregivers. So this is a massive issue that is not going to go away.
The other thing that is changing is that in low-income countries, just as in high-income countries, there used to be a great reliance on family carers and often older people are now alone.
What difference can a U.N. declaration make on the ground for families dealing with dementia?
We have reports from all over the world of people in distress, in angst, with massive mental health issues [because they or their family member has dementia]. And it is difficult if you are alone facing this. And if the community around them doesn’t know what’s happening, they can exclude you rather than include you, and that can become an extra burden. In our survey last year, we found out that a lot of carers — about 33% — stopped doing any social activity after a diagnosis, because they’re ashamed and they don’t know how to communicate [about dementia].
Even at the highest level of government, dementia has so far been excluded. This U.N. declaration, for us, is really important because people now will be able to say: ‘No, no. We are a major non- communicable disease.’
But it’s just one step and I am under no illusions. Getting [a dementia action plan] implemented country by country is going to take years — decades, maybe even.
What does that look like for lower-income countries, especially where health budgets are already tight?
[In some higher-income countries, there are medications on the market that aim to help] but, right now, we are aware that that’s not possible [in many lower-income countries].
In some countries, the infrastructure and regulatory approval is not there. The testing and diagnostic capacity are not there. Even the medical professionals — the psychiatrist, the neurologist, the geriatricians — are not there. And some of the treatments currently available are very expensive. Some countries can simply not afford them.
But it’s not just medications that matter.
We were particularly keen for people to understand that you can live a better life if you can have better care. Many families report that once they get a diagnosis, they are left absolutely alone with no information whatsoever. But there can be basic helplines, basic support groups.
There is only so much that civil society can do. This is about the government being conscious of the fact that this is a societal challenge. They have to embrace it just the way they’ve embraced other conditions, like cancer or heart disease. And ask questions like: How can it be integrated in our health care system? How much money can go towards it?
However, as [with] everything that has to do with the U.N. it could remain just as a piece of paper. We need to make sure that there is implementation, that governments put in place public health campaigns that include dementia. We will do a lot of work to make sure that this becomes tangible for the people that live with dementia and for their families.
Supreme Court appears split in tax foreclosure case
At issue is whether a county can seize homeowners' residence for unpaid property taxes and sell the house at auction for less than the homeowners would get if they put their home on the market themselves.
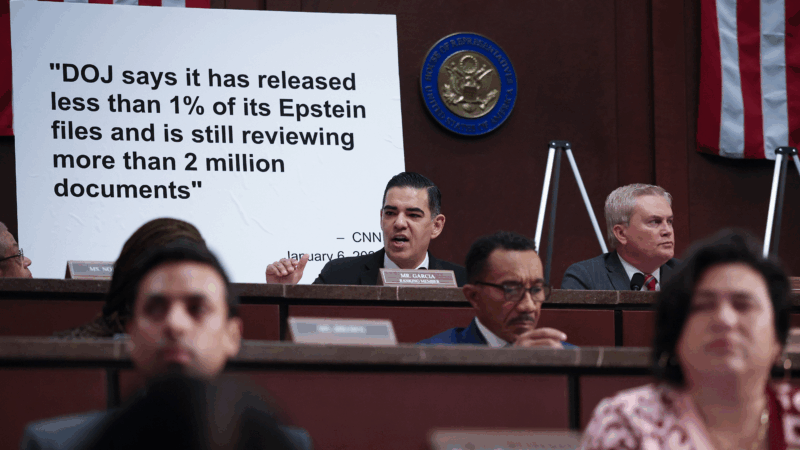
Top House Dem wants Justice Department to explain missing Trump-related Epstein files
After NPR reporting revealed dozens of pages of Epstein files related to President Trump appear to be missing from the public record, a top House Democrat wants to know why.
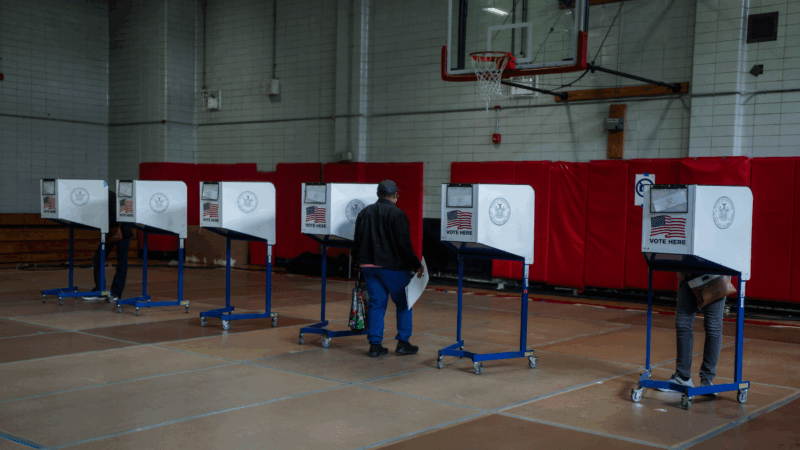
ICE won’t be at polling places this year, a Trump DHS official promises
In a call with top state voting officials, a Department of Homeland Security official stated unequivocally that immigration agents would not be patrolling polling places during this year's midterms.
Cubans from US killed after speedboat opens fire on island’s troops, Havana says
Cuba says the 10 passengers on a boat that opened fire on its soldiers were armed Cubans living in the U.S. who were trying to infiltrate the island and unleash terrorism. Secretary of State Marco Rubio says the U.S. is gathering its own information.
Surgeon general nominee Means questioned about vaccines, birth control and financial conflicts
During a confirmation hearing, senators asked Dr. Casey Means about her current positions and her past statements on a range of public health issues.
Rock & Roll Hall of Fame 2026 shortlist includes Lauryn Hill, Shakira and Wu-Tang Clan
The shortlist also includes a 1990s pop diva, heavy metal pioneers and a legendary R&B singer and producer.