Research suggests doctors might quickly become dependent on AI
Artificial intelligence is beginning to help doctors screen patients for several routine diseases. But a new study raises concerns about whether doctors might become too reliant on AI.
The study looking at gastroenterologists in Poland found that they appeared to be about 20% worse at spotting polyps and other abnormalities during colonoscopies on their own, after they’d grown accustomed to using an AI-assisted system.
The findings, published in the journal Lancet Gastroenterology and Hepatology, suggest that even after a short period of using AI, experts may become overly dependent on AI to do certain aspects of their jobs.
“We were quite surprised,” says Marcin Romańczyk, an M.D.-Ph.D. gastroenterologist at H-T Medical Center in Tychy, Poland, who led the study.
But not everyone is convinced that the paper proves doctors are losing critical skills because of AI.
“I think three months seems like a very short period to lose a skill that you took 26 years to build up,” says Johan Hulleman, a researcher at Manchester University in England who has studied human reliance on artificial intelligence.
Hulleman believes statistical variations in the patient data might be part of the explanation for why the numbers appear to drop. Factors such as the average age of the patients used in different sections of the study might explain the variation, he says.
AI in medicine
Artificial intelligence is becoming increasingly common for a number of routine medical scans. The next time you get a scan for your eyes, breast cancer, or colon disease, there’s a decent chance that AI might be analyzing the images.
“AI is spreading everywhere,” Romańczyk says. At the same time, many doctors are playing catch-up, because learning how to use the technology wasn’t part of their training.
“We’ve been taught from books and from our teachers,” he says. “No one told us how to use AI.”
A few years ago, four clinics in Poland tried out an AI system to detect polyps and other abnormalities during colonoscopies. The AI works in real time, analyzing video from a camera inside the colon.
If it spots something, it will highlight the area for the clinician to see.
“In this particular one there’s a green box, showing where the polyp might be,” he says.
In the box
The clinics were collecting data on whether the AI system worked. It turns out it did, but when Romańczyk and his colleagues reanalyzed the data, they found something else: After the system was introduced, doctors became significantly worse at detecting possible polyps when the AI was switched off.
According to their analysis, after doctors got AI, detection rates of possible polyps fell from 28.4% to 22.4% when their new AI system was switched off. In other words, the doctors seemed to become quickly dependent on AI systems catching the polyps. Romańczyk says he’s not quite sure why it’s happening, but he has some theories.
“We are subconsciously waiting for the green box to come out to show us the region where the polyp is and we’re not paying so much attention,” he says.
There are other examples that support that idea: A similar study has shown that nonexperts do a worse job scanning mammograms if they know they can get an AI system to help them with the push of a button.
Johan Hulleman, who helped lead that mammogram study, describes it as a “safety-net effect.” He says these latest results could be interesting, but he’s skeptical. The study of colonoscopies took place over three months, and the doctors participating had decades of experience. He thinks statistical variations due to a number of factors, such as age of the patients, might be behind the apparent drop.
Additionally, he says, “We don’t know how many polyps there really were, so we don’t know the ground truth.” By that he means it’s unclear how many of the possible polyps that doctors supposedly missed were actually medically important.
The study’s author, Romańczyk, does believe the drop is real — though he admits that studying AI in a clinical setting like this can be tricky. There are a lot of variables the researchers couldn’t control.
He’s not against using AI. He actually thinks the little green boxes help him to do better colonoscopies. But he thinks that there should be more studies like these examining how AI might be changing the way doctors work in the real world.
“Because look what’s happening,” he says. “We have AI systems that are available, but we don’t have the data.”
Transcript:
MARY LOUISE KELLY, HOST:
Artificial intelligence is showing up at the doctor’s office. AI algorithms are beginning to help screen for several routine diseases. But as NPR’s Geoff Brumfiel reports, a new study is raising concerns about whether doctors might become too reliant on AI.
GEOFF BRUMFIEL, BYLINE: The next time you get a scan for your eyes, breast cancer or colon disease, there’s a decent chance that artificial intelligence might be analyzing the images.
MARCIN ROMANCZYK: AI is spreading everywhere.
BRUMFIEL: Marcin Romanczyk is a doctor at H-T. Medical Center in Tychy, Poland. He says although AI is moving rapidly into medicine, many doctors are playing catch-up. It simply wasn’t part of their training.
ROMANCZYK: All the doctors – we’ve been taught from books and from our teachers. No one told us how to use AI.
BRUMFIEL: Romanczyk is a gastroenterologist. A few years ago, several clinics in Poland tried out an AI system to detect polyps during colonoscopies. The AI works in real time, analyzing video from a camera inside the colon. If it spots something…
ROMANCZYK: We see some kind of marking. In this particular one, there’s a green box showing where the polyp might be.
BRUMFIEL: The clinics were collecting data on whether the AI worked. It turns out it did. But when Romanczyk and his colleagues reanalyzed the data, they found something else. After the system was introduced, doctors became significantly worse at detecting possible polyps when the AI was switched off.
ROMANCZYK: We were quite actually surprised.
BRUMFIEL: According to a new analysis published in the journal, Lancet Gastroenterology And Hepatology, after doctors got AI, detection rates without it fell by roughly 20%. In other words, the doctors seem to become quickly dependent on AI systems catching the polyps. Romanczyk says he’s not quite sure why it’s happening, but he has some theories.
ROMANCZYK: We are subconsciously waiting for the green box to come out and show us the region where the polyp is, and we are not paying so much attention.
BRUMFIEL: There are some other examples that support that idea. A similar study has shown that people do a worse job scanning mammograms if they know they can get an AI system to help them with the push of a button. Johan Hulleman is a researcher at Manchester University in the U.K. who helped lead that mammogram study. He says these latest results could be interesting, but he’s a little skeptical. The study took place over three months and the doctors participating had decades of experience.
JOHAN HULLEMAN: I think three months kind of – it seems a very short period to lose the skill that you took, like, 26 years to build up.
BRUMFIEL: He thinks statistical variations due to a number of factors might be making the drop look larger than it is.
HULLEMAN: We don’t know how many polyps there really were. And so we don’t know the grand truth.
BRUMFIEL: By that, he means it’s unclear how many of the possible polyps were medically important. The study’s author, Romanczyk, does believe the drop is real, though he admits studying AI in a clinical setting like this can be tricky. There are a lot of variables the researchers couldn’t control. And that’s why Romanczyk thinks that there should be more studies like these, looking at how AI might be changing the way doctors work in the real world.
ROMANCZYK: Because look what’s happening. We have AI systems that they are available, but we don’t have the data.
BRUMFIEL: About how doctors interact with those systems. He’s not against using AI. He actually thinks the little green boxes help him do better colonoscopies. He just wants to make sure this rapid rollout of a new technology is supported by facts, not just feels.
Geoff Brumfiel, NPR News.
(SOUNDBITE OF MUSIC)
Trump and Netanyahu to meet in Florida at a crucial moment for the Gaza ceasefire
President Trump could use the face-to-face at his Mar-a-Lago estate to look for ways to speed up the peace process, as Israel's leader has been accused of not pushing his side to move fast enough.
‘Bomb cyclone’ forecasted to bring heavy snow, blizzard conditions and dangerous travel
A 'bomb cyclone' is intensifying severe winter weather for millions of people across the U.S. The system is expected to knock out power and disrupt holiday travel.
Russia sends 3 Iranian satellites into orbit, report says
The report said that a Russian rocket sent the satellites on Sunday from a launchpad in eastern Russia.
Viral global TikToks: A twist on soccer, Tanzania’s Charlie Chaplin, hope in Gaza
TikToks are everywhere (well, except countries like Australia and India, where they've been banned.) We talk to the creators of some of the year's most popular reels from the Global South.
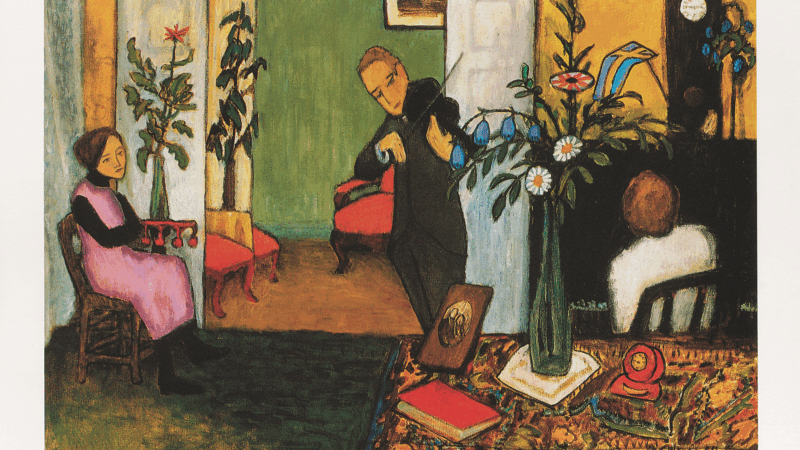
This painting is missing. Do you have it?
An important work from a rediscovered artist has been absent from public view since the 1970s. A New York curator is hunting for it.
Memory loss: As AI gobbles up chips, prices for devices may rise
Demand for memory chips currently exceeds supply and there's very little chance of that changing any time soon. More chips for AI means less available for other products such as computers and phones and that could drive up those prices too.