How Dr. Emily Fortney is using her clinical psychology work to help pregnant people
Suicide rates are rising for pregnant people, especially Black mothers and those who are living in poverty.
Dr. Emily Fortney has been a clinical psychologist for nearly a decade, but she recently combined her work in mood disorders and mania with her personal experiences in maternal care to create a framework of care for mothers who are struggling with perinatal mental health issues. She currently offers services to families in Mississippi, California and Virginia.
She spoke with The Gulf States Newsrooms’ Maya Miller on what she’s seeing in her private practice as suicide rates continue to rise.
The following conversation has been condensed and edited for clarity.

It wasn’t really until about two years ago after I went through a pretty traumatic miscarriage at 20 weeks and then went on to have my son where I really had a pull to incorporating perinatal mental health into my private practice. So that’s kind of my why. Um, I was in Mississippi at the time and just really noticing throughout my treatment and kind of my care the lack of kind of knowledge about perinatal mood and anxiety disorders and how to treat them, how to screen for them. And so that led me to getting certified in perinatal mental health. Most of my clinical work has been with, I would say, more serious and complex mental health needs, like suicidality, psychosis, you know, mania, things of that nature. And so I’m now kind of bringing and blending that work with my role with new moms.
What sorts of trends are you seeing in, like your research and your practice, you know, with the types of parents that you’re seeing or the backgrounds of families that you’re working with?
Within my own practice, what I’ve been seeing is an increase. You know, a lot of women coming to me that have perinatal mood and anxiety disorders that were not detected and not diagnosed during pregnancy or postpartum. And I’m seeing more and more of kind of suicidal ideation that we’re having to screen and assess for and manage.
You mentioned risk factors for suicidality. What are some of those risk factors?
Some of those risk factors are obviously having a previous diagnosis of depression or anxiety, having a history of any other perinatal mood and anxiety disorders, any kind of history of abuse or like childhood abuse or even intimate partner violence is another risk factor. And then another big one is substance use and then sleep deprivation.
And so how do you feel stigma around needing mental health care affects new moms?
Oh, I think stigma is huge. I think that is something we’ve been battling for a long time. I will say that, you know, I think, with where there is a plus with social media is that it’s helping reduce a lot of the stigmas. But I think also with social media, we are romanticizing pregnancy and motherhood in a lot of ways, and that is increasing the stigma and decreasing people accessing care because they feel ashamed or embarrassed.
Yeah, it’s interesting that you say like romanticizing motherhood because, you know, if you’re feeling unsupported in your home, then you’re kind of afraid to reach out to other people because you want to make sure that you’re giving this illusion that everything’s gravy.
Absolutely. Absolutely. And I think even more so, just with motherhood and like post-birth, like there’s this expectation that these are the happiest days of your life. And there’s pressure. Like, enjoy every moment. You know, the days are long, but the years are short, when really the day-to-day reality is that women and childbearing persons are under a lot of pressure and even more so pressure now because of social media, because we’re living in a post-pandemic world and society, and the U.S. is still behind when it comes to maternal health and maternal mental health care.
That sort of segues into my next question about a 2020 study of insured mothers found that mothers who are on Medicaid may be at a higher risk of suicide. And in Mississippi, Medicaid coverage runs out at like two months, even though they’re still at a higher risk for suicide in that first year. Nearby states have expanded, you know, postpartum Medicaid for up to a year. Do you think that that’s one solution here for maternal mental health?
That is one of the many ways where we can start detecting things early on through screeners having more face-to-face interactions like with moms and checking in on them. You know, I think it’s a great first step in a very multi-layered situation that we need more, we need better care and we need better care that entire first year at a minimum.
So there are a lot of different factors that, you know, come into play. And, you know, it’s a very nuanced sort of solution because, you know, something that works for one mom may not work for another mom based on their preexisting sort of issue.
Yes, exactly. And that’s where screening and assessment is really important. And we still don’t have a universal kind of system for that right now, like in our doctor’s offices, and that’s where integrated care becomes really important with mental health and like physicians, because every woman is coming in with a unique background and unique story and we need to take each one very seriously.
If you or someone you know is struggling with suicidal thoughts or actions, please call the National Suicide Prevention Hotline at 988. The Crisis Help Line is also available for emotional support. Text HELLO to 74174 to speak with a trained listener.
This story was produced by the Gulf States Newsroom, a collaboration among Mississippi Public Broadcasting, WBHM in Alabama and WWNO and WRKF in Louisiana and NPR. Support for reproductive health coverage comes from the Commonwealth Fund.
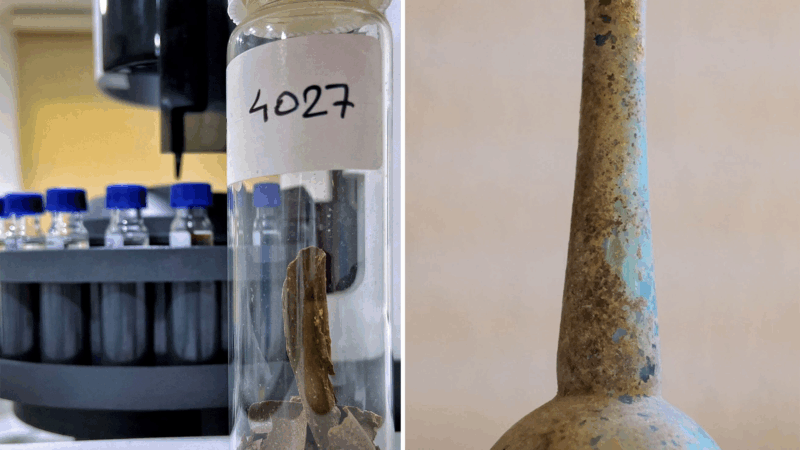
That ain’t perfume! Ancient bottle contained feces, likely used for medicine
Researchers found a tiny bottle from ancient Rome that contained fecal residue and traces of aromatics, offering evidence that poop was used medicinally more than 2,000 years ago.
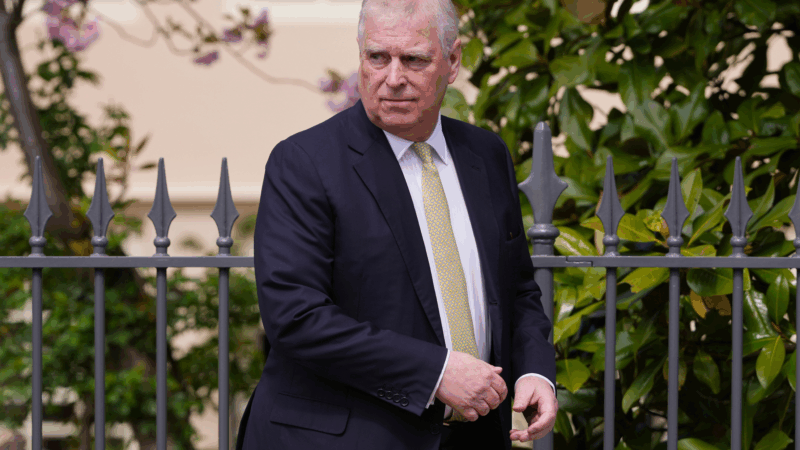
Britain’s former Prince Andrew arrested on suspicion of misconduct in public office
Andrew Mountbatten-Windsor, formerly Prince Andrew, has been arrested on suspicion of misconduct in public office.
Urban sketchers find the sublime in the city block
Sketchers say making art together in urban environments allows them to create a record of a moment and to notice a little bit more about the city they see every day.
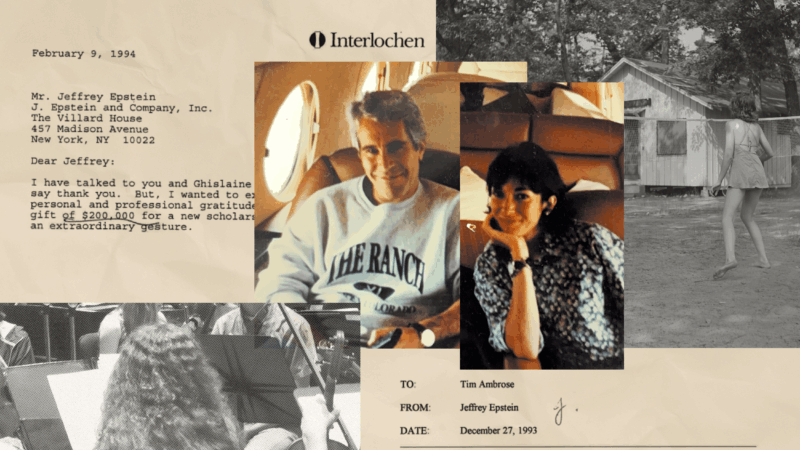
Epstein once attended an elite arts camp. Years later, he used it to find his victims
Jeffrey Epstein and Ghislaine Maxwell lavished money on the Interlochen Center for the Arts to gain access, documents show — even funding an on-campus lodge they stayed in. In the process, two teenagers were pulled into their orbit.
How a recent shift in DNA sleuthing might help investigators in the Nancy Guthrie case
DNA science has helped solve criminal cases for decades. But increasingly, investigative genetic genealogy — which was first used for cold cases — is helping to solve active cases as well.
An unsung hero stepped in to help a newly widowed mom in a moment of need
Barbara Alvarez lost her husband in 2017, just before their daughter went off to college. Her unsung hero helped her find the strength to be a single mother to her child at a key moment in their lives.