UAB Researchers Develop New Way to Create Stem Cells
Researchers at UAB have found a new way to create stem cells, one they hope will lead to more efficient and personalized medical treatments. The findings were published Tuesday in Cell Reports.
“In humans, we have more than 200 types of cells,” says Kejin Hu, lead researcher and an assistant professor at the UAB Stem Cell Institute. “But [in] all of these 200 types of cells, they contain the same generic material.”
While there are thousands of genes, any individual cell only expresses some of them. The particular combination of genes determines whether the cell is skin or muscle, for instance.
That process of gene expression starts through what’s called transcription. Transcription is kind of the cell’s way of “reading” the genetic information before going on to do something with it. It’s routine and ongoing, but transcription hits pause when the cell divides.
“How does the cell remember which gene is active, which gene is silenced?” says Hu. “How does the transcription machinery go back to the right place?”
Hu says the cell has protein “bookmarks” so it knows where to pick up after it divides. But instead of allowing the cells to continue on their way, researchers can use chemicals to target these bookmarks and remove them. It’s as if the cell’s memory is wiped clean.
Scientists already knew they could target these bookmarks. But what Hu’s research shows is that once they were gone, cells could more easily be “reprogramed” into another type. They become stem cells.
A Simpler Way
This is not the only way to make stem cells, but Hu says this method is a better than current practices.
Embryonic stem cells come from human embryos. As a result, their use in research generates ethical controversy. Scientists can also create stem cells by transplanting the nucleus of an adult cell into an egg cell. But Hu says this method is technically difficult and only a few labs are capable of performing it successfully.
Hu says targeting the transcriptional bookmarks is simpler and could go a long way to developing personal medical therapies from a individual’s own cells. In theory, doctors could grow tissue or organs and heal our bodies like we repair cars. Using the reprogrammed cells from the patient would also eliminate the risk of rejection that comes with embryonic stem cells.
But Hu cautions we’re nowhere near that yet. He says reprogramming human cells is not efficient enough at this point to use clinically. It also takes more time than the nuclear transfer method.
“We still have a long way as a therapy,” says Hu. “We need a lot of improvement.”
Supreme Court appears split in tax foreclosure case
At issue is whether a county can seize homeowners' residence for unpaid property taxes and sell the house at auction for less than the homeowners would get if they put their home on the market themselves.
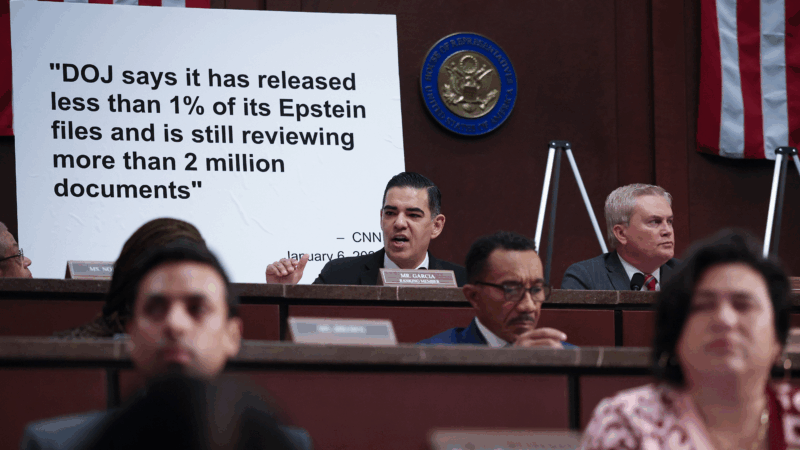
Top House Dem wants Justice Department to explain missing Trump-related Epstein files
After NPR reporting revealed dozens of pages of Epstein files related to President Trump appear to be missing from the public record, a top House Democrat wants to know why.
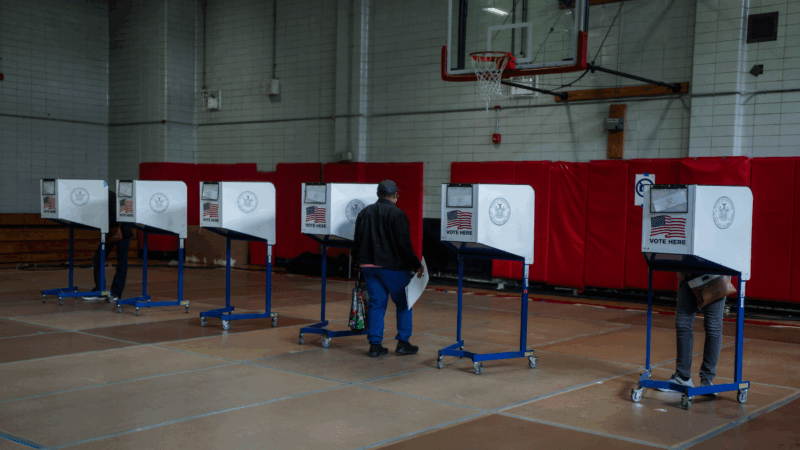
ICE won’t be at polling places this year, a Trump DHS official promises
In a call with top state voting officials, a Department of Homeland Security official stated unequivocally that immigration agents would not be patrolling polling places during this year's midterms.
Cubans from US killed after speedboat opens fire on island’s troops, Havana says
Cuba says the 10 passengers on a boat that opened fire on its soldiers were armed Cubans living in the U.S. who were trying to infiltrate the island and unleash terrorism. Secretary of State Marco Rubio says the U.S. is gathering its own information.
Surgeon general nominee Means questioned about vaccines, birth control and financial conflicts
During a confirmation hearing, senators asked Dr. Casey Means about her current positions and her past statements on a range of public health issues.
Rock & Roll Hall of Fame 2026 shortlist includes Lauryn Hill, Shakira and Wu-Tang Clan
The shortlist also includes a 1990s pop diva, heavy metal pioneers and a legendary R&B singer and producer.