Why so many clinics that provide abortion are closing, even where it’s still legal
On the last day of patient care at the Planned Parenthood clinic in Marquette, Mich., a port town on the shore of Lake Superior, dozens of people crowded into the parking lot and alley, holding pink homemade signs that read “Thank You!” and “Forever Grateful.”
“Oh my god,” physician assistant Anna Rink gasped, as she and three other Planned Parenthood employees finally walked outside. The crowd whooped and cheered. Then Rink addressed the gathering.
“Thank you for trusting us with your care,” Rink called out, her voice quavering. “And I’m not stopping here. I’m only going to make it better. I promise. I’m going to find a way.”
“We’re not done!” someone called out. “We’re not giving up!”
But Planned Parenthood of Michigan is giving up on four of its health centers in the state, citing financial challenges.
That includes the one in Marquette, the only clinic that provided abortion in the vast, sparsely populated Upper Peninsula. For the roughly 1,100 patients who visited the clinic each year for anything from cancer screenings to contraceptive implants, the next-closest Planned Parenthood will now be a nearly five-hour drive south.
It’s part of a growing trend: At least 17 clinics closed last year in states where abortion remains legal, and another 17 have closed in just the first five months of this year, according to data gathered by ineedana.com. That includes states that have become abortion destinations, like Illinois, and those where voters have enshrined broad reproductive rights into the state constitution, like Michigan.
Experts say the closures indicate that financial and operational challenges, rather than future legal bans, may be the biggest threats to abortion access in states whose laws still protect it.
“These states that we have touted as being really the best kind of versions of our vision for reproductive justice, they too struggle with problems,” said Erin Grant, a co-executive director of the Abortion Care Network, a national membership organization for independent clinics.
“It’s gotten more expensive to provide care, it’s gotten more dangerous to provide care, and it’s just gotten, frankly, harder to provide care, when you’re expected to be in the clinic and then on the statehouse steps, and also speaking to your representatives and trying to find somebody who will fix your roof or paint your walls who’s not going to insert their opinion about health care rights.”
But some abortion-rights supporters question whether leaders are prioritizing patient care for the most vulnerable populations. Planned Parenthood of Michigan isn’t cutting executive pay, even as it reduces staff by 10% and shuts down brick-and-mortar clinics in areas already facing health care shortages.

“I wish I had been in the room so I could have fought for us and I could have fought for our community,” said Viktoria Koskenoja, an emergency medicine physician in the Upper Peninsula, who previously worked for Planned Parenthood in Marquette.
“I just have to hope that they did the math of trying to hurt as few people as possible and that’s how they made their decision. And we just weren’t part of the group that was going to be saved,” Koskenoja said.
Why clinics are closing now, three years after Roe was overturned
If a clinic could survive the fall of Roe v. Wade, “you would think that resilience could carry you forward,” said Brittany Fonteno, president and CEO of the National Abortion Federation.
But clinic operators say they face new financial strain, including rising costs, limited reimbursement rates and growing demand for telehealth services.
Clinics are also bracing for the Trump administration to again exclude them from Title X, the federal funding for low- and no-cost family planning services, as the previous Trump administration did in 2019.
Planned Parenthood of Michigan (PPMI) says the cuts are painful but necessary for the organization’s long-term sustainability.
The four clinics being closed are “our smallest health centers,” said Sarah Wallett, PPMI’s chief medical operating officer. While the thousands of patients those clinics served each year are important, she said, the clinics’ small size made them “the most difficult to operate.”
The clinics being closed had offered medication abortion, which is available in Michigan up until 11 weeks of pregnancy, but not procedural abortion.
Planned Parenthood of Illinois (a state that has become a post-Roe v. Wade abortion destination) shuttered four clinics in March, pointing to a “financial shortfall.”
Planned Parenthood of Greater New York is now selling its only Manhattan clinic, after closing four clinics elsewhere in the state last summer due to “compounding financial and political challenges.”
Planned Parenthood Association of Utah, where courts have blocked a near-total abortion ban and where abortion is currently legal until 18 weeks of pregnancy, announced it will close two centers in May.
This spring, the Trump administration began temporarily freezing funds to many clinics, including all Title X providers in California, Hawaii, Maine, Mississippi, Missouri, Montana and Utah, according to a KFF analysis.
While the current Title X freeze doesn’t yet include Planned Parenthood of Michigan, PPMI’s chief advocacy officer, Ashlea Phenicie, said it would amount to a loss of about $5.4 million annually, or 16% of its budget.
But Planned Parenthood of Michigan didn’t shut down any clinics the last time the Trump administration froze its Title X funding. Leaders said that’s because the funding was stopped for only about two years, from 2019 until 2021, when the Biden administration restored it.
“Now we’re faced with a longer period of time that we will be forced out of Title X, as opposed to the first administration,” said PPMI President and CEO Paula Thornton Greear.
At the same time, the rise of telehealth abortion has put “new pressures in the older-school, brick-and-mortar facilities,” said Caitlin Myers, a Middlebury College economics professor who maps brick-and-mortar abortion clinics across the United States.
Balancing cost and care
Until a few years ago, doctors could prescribe abortion pills only in person. Those restrictions were lifted during the pandemic, but it was the Dobbs decision in 2022 that really “accelerated expansions in telehealth,” Myers said. “Because it drew all this attention to models of providing abortion services.”
Suddenly, new online providers entered the field, advertising virtual consultations and pills shipped directly to your home. And plenty of patients who still have access to a brick-and-mortar clinic prefer that option. “Put more simply, it’s gotta change their business model,” she said.

Historically, about 28% of PPMI’s patients receive Medicaid benefits, according to Phenicie. And like many states, Michigan’s Medicaid program doesn’t cover abortion, leaving those patients to either pay out-of-pocket or rely on help from abortion funds, several of which have also been struggling financially.
“When patients can’t afford care, that means that they might not be showing up to clinics,” said Fonteno of the National Abortion Federation, which had to cut its monthly budget nearly in half last year, from covering up to 50% of an eligible patient’s costs to 30%.
“So seeing a sort of decline in patient volume, and then associated revenue, is definitely something that we’ve seen,” Fonteno said.
Meanwhile, more clinics and abortion funds say patients have delayed care because of those rising costs. According to a small November-December 2024 survey of providers and funds conducted by ineedana.com, “85% of clinics reported seeing an increase of clients delaying care due to lack of funding.”
One abortion fund said the number of patients who’ve had to delay care until their second trimester “has grown by over 60%” spanning six months in 2024.

Even when non-abortion services like birth control and cervical cancer screenings are covered by insurance, clinics aren’t always reimbursed for the full cost, Thornton Greear said.
“The reality is that insurance reimbursement rates across the board are low,” she said. “It’s been that way for a while. When you start looking at the costs to run a health care organization, from supply costs, etc., when you layer on these funding impacts, it creates a chasm that’s impossible to fill.”
Yet, unlike some independent clinics that have had to close, Planned Parenthood’s national federation brings in hundreds of millions of dollars a year, the majority of which is spent on policy and legal efforts rather than state-level medical services.
The organization and some of its state affiliates have also battled allegations of mismanagement, as well as complaints about staffing and patient care problems. Planned Parenthood of Michigan staffers in five clinics unionized last year, with some citing management problems and workplace and patient care conditions.
Asked whether Planned Parenthood’s national funding structure needs to change, PPMI CEO Thornton Greear said: “I think that it needs to be looked at, and what they’re able to do. And I know that that is actively happening.”
The gaps that telehealth can’t fill
When the Marquette clinic’s closure was announced, dozens of patients voiced their concerns in Google reviews, with several saying the clinic had “saved my life,” and describing how they’d been helped after an assault, or been able to get low-cost care when they couldn’t afford other options.
Planned Parenthood of Michigan responded to most comments with the same statement and pointed patients to telehealth in the clinic’s absence:
“Please know that closing health centers wasn’t a choice that was made lightly, but one forced upon us by the escalating attacks against sexual and reproductive health providers like Planned Parenthood. We are doing everything we can to protect as much access to care as possible. We know you’re sad and angry — we are, too.
“We know that telehealth cannot bridge every gap; however, the majority of the services PPMI provides will remain available via the Virtual Health Center and PP Direct, including medication abortion, birth control, HIV services, UTI treatment, emergency contraception, gender-affirming care, and yeast infection treatment. Learn more at ppmi.org/telehealth.”
PPMI’s virtual health center is already its most popular clinic, according to the organization, serving more than 10,000 patients a year. And PPMI plans to expand virtual appointments by 40%, including weekend and evening hours.
“For some rural communities, having access to telehealth has made significant changes in their health,” said Wallett, PPMI’s chief medical operating officer. “In telehealth, I can have an appointment in my car during lunch. I don’t have to take extra time off. I don’t have to drive there. I don’t have to find child care.”
Yet even as the number of clinics has dropped nationally, brick-and-mortar facilities still account for about 80% of clinician-provided abortions, according to the most recent #WeCount report looking at April-June 2024.
Hannah Harriman, a Marquette County Health Department nurse who previously spent 12 years working for Planned Parenthood of Marquette, is skeptical of any suggestion that telehealth can replace a rural brick-and-mortar clinic. “I say that those people have never spent any time in the U.P.,” she said, referring to the Upper Peninsula.
Some areas are “dark zones” for cell coverage, she said. And some residents “have to drive to McDonald’s to use their Wi-Fi. There are places here that don’t even have internet coverage. I mean, you can’t get it.”
Telehealth has its advantages, said Koskenoja, the emergency medicine physician who previously worked for Planned Parenthood in Marquette, “but for a lot of health problems, it’s just not a safe or realistic way to take care of people.”
She recently had a patient in the emergency room who was having a complication from a gynecological surgery. “She needed to see a gynecologist, and I called the local OB office,” Koskenoja said. “They told me they have 30 or 40 new referrals a month,” and simply don’t have enough clinicians to see all those patients. “So adding in the burden of all the patients that were being seen at Planned Parenthood is going to be impossible.”
Koskenoja, Harriman, and other local health care providers have been strategizing privately to figure out what to do next to help people access everything from Pap smears to IUDs. The local health department can provide Title X family planning services 1½ days a week, but that won’t be enough, Harriman said.
And there are a few private “providers in town that offer medication abortion to their patients only — very, very quietly,” Harriman said. But that won’t help patients who don’t have good insurance or are stuck on waitlists.
“It’s going to be a patchwork of trying to fill in those gaps,” Koskenoja said. “But we lost a very functional system for delivering this care to patients. And now, we’re just having to make it up as we go.”
This story comes from NPR’s health reporting partnership with Michigan Public and KFF Health News.
Transcript:
MICHEL MARTIN, HOST:
Some clinics that offer abortion are closing their doors, even in states where abortion is still legal. It’s happening in New York, Illinois, in Utah and now in Michigan, where voters passed a constitutional amendment in 2022 protecting abortion rights. Planned Parenthood of Michigan closed four brick-and-mortar clinics last month, including the last remaining clinic in the rural Upper Peninsula. Kate Wells from member station Michigan Public reports that reproductive health care is facing new financial pressures.
KATE WELLS, BYLINE: On the last day, they saw patients at the Planned Parenthood in Marquette, Michigan, a port town on the shore of Lake Superior, dozens of people lined up outside. They held handmade pink signs that said Thank You and Grateful For You. And when the small clinical team finally exited the building…
(SOUNDBITE OF ARCHIVED RECORDING)
UNIDENTIFIED PERSON #1: Off they go (ph).
WELLS: …The crowd erupted in cheers.
(CHEERING)
WELLS: We’re not done, someone shouted.
(SOUNDBITE OF ARCHIVED RECORDING)
UNIDENTIFIED PERSON #2: We’re not done.
WELLS: We’re not giving up.
(SOUNDBITE OF ARCHIVED RECORDING)
UNIDENTIFIED PERSON #2: We’re not giving up.
WELLS: Finally, Planned Parenthood physician assistant Anna Rink addressed the crowd.
(SOUNDBITE OF ARCHIVED RECORDING)
ANNA RINK: I’m not leaving this community. I’m not leaving this camp. I’m not giving up on this dream. It’s going to continue. It’s going to grow. We’re going to build it and make it better. I promise.
WELLS: But Planned Parenthood of Michigan is giving up on this clinic, the only clinic in the Upper Peninsula offering abortion. They’re also shutting down three other health centers in the state. Dr. Sarah Wallett is their chief medical operating officer.
SARAH WALLETT: Our smallest health centers, those patients are important. Their health care is important, but operationally, because of their small size, are the most difficult to operate.
WELLS: Instead, Planned Parenthood of Michigan is encouraging many of those patients to turn to telehealth. Their organization’s virtual clinic is expanding, and it already sees more than 10,000 Michigan patients a year.
WALLETT: In telehealth, I can have an appointment in my car during lunch. I don’t have to take extra time off. I don’t have to drive there. I don’t have to find child care.
WELLS: And this is a big shift because until just a few years ago, doctors could only prescribe abortion pills in person. That requirement was lifted because of COVID, but telehealth abortion really took off in 2022, when the Supreme Court overturned Roe v. Wade with the Dobbs ruling. Caitlin Myers is an economics professor at Middlebury College.
CAITLIN MYERS: And Dobbs almost paradoxically accelerated expansions in telehealth because it drew all this attention to models of providing abortion services.
WELLS: Myers tracks every brick-and-mortar abortion clinic in the U.S., and she says, suddenly, after Dobbs, you could just get pills shipped directly to your home as long as you were in your first 11 weeks of pregnancy. And that appealed to a lot of patients, including those who might otherwise go to traditional clinics.
MYERS: That’s going to create new pressures on kind of the older-school brick-and-mortar facilities. I think, put more simply, it’s got to change their business model.
WELLS: At the same time, running an in-person clinic is getting harder financially. Although donors have stepped up after the Dobbs decision, since then, fundraising has slowed. And Planned Parenthood is expecting the Trump administration to once again exclude its clinics from Title X funding. That is the federal money for medical providers who do free and low-cost family planning. So Planned Parenthood of Michigan is leaning into telehealth. But Hannah Harriman is skeptical.
HANNAH HARRIMAN: I say that those people have not spent any time in the UP.
WELLS: That’s the Upper Peninsula. Harriman is a public health nurse there at the Marquette County Health Department. She previously worked for 12 years at the Planned Parenthood that is closing. And she says some of those patients simply won’t be able to access telehealth.
HARRIMAN: There are people that have to drive to McDonald’s to use their WiFi. There are places here that don’t even have internet coverage. I mean, you can’t get it.
WELLS: And she says, even for the patients who can get virtual care, it’s limited. Telehealth can’t give you an ultrasound or insert an IUD. And she says you lose the human touch, the stuff that was her favorite part of the job.
HARRIMAN: Sometimes you cry with them and you laugh with them. And then when they have that trust, they keep coming back for care.
WELLS: Now the closest Planned Parenthood will be a nearly five-hour drive south. And Harriman says that is just not a trip that every patient will be able to make.
HARRIMAN: There’s going to be an increase in undetected cervical cancers, many more unplanned pregnancies. Lots of families are going to suffer.
WELLS: For patients, it doesn’t really matter why a clinic closes, whether it’s a legal ban or a funding cut. Either way, it can make the care that they need that much harder to get.
For NPR News, I’m Kate Wells in Ann Arbor, Michigan.
MARTIN: This story comes from NPR’s partnership with Michigan Public and KFF Health News.
Mideast clashes breach Olympic truce as athletes gather for Winter Paralympic Games
Fighting intensified in the Middle East during the Olympic truce, in effect through March 15. Flights are being disrupted as athletes and families converge on Italy for the Winter Paralympics.
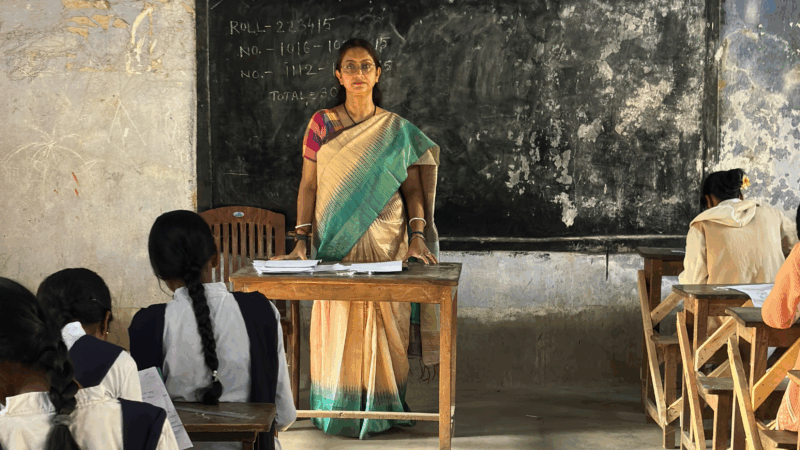
A U.S. scholarship thrills a teacher in India. Then came the soul-crushing questions
She was thrilled to become the first teacher from a government-sponsored school in India to get a Fulbright exchange award to learn from U.S. schools. People asked two questions that clouded her joy.
Sunday Puzzle: Sandwiched
NPR's Ayesha Rascoe plays the puzzle with WXXI listener Jonathan Black and Weekend Edition Puzzlemaster Will Shortz.
U.S.-Israeli strikes in Iran continue into 2nd day, as the region faces turmoil
Israel said on Sunday it had launched more attacks on Iran, while the Iranian government continued strikes on Israel and on U.S. targets in Gulf states, Iraq and Jordan.
Trump warns Iran not to retaliate after Ayatollah Ali Khamenei is killed
The Iranian government has announced 40 days of mourning. The country's supreme leader was killed following an attack launched by the U.S. and Israel on Saturday against Iran.
Iran fires missiles at Israel and Gulf states after U.S.-Israeli strike kills Khamenei
Iran fired missiles at targets in Israel and Gulf Arab states Sunday after vowing massive retaliation for the killing of Supreme Leader Ayatollah Ali Khamenei by the United States and Israel.