For those with addiction, going into and coming out of prison can be a minefield.
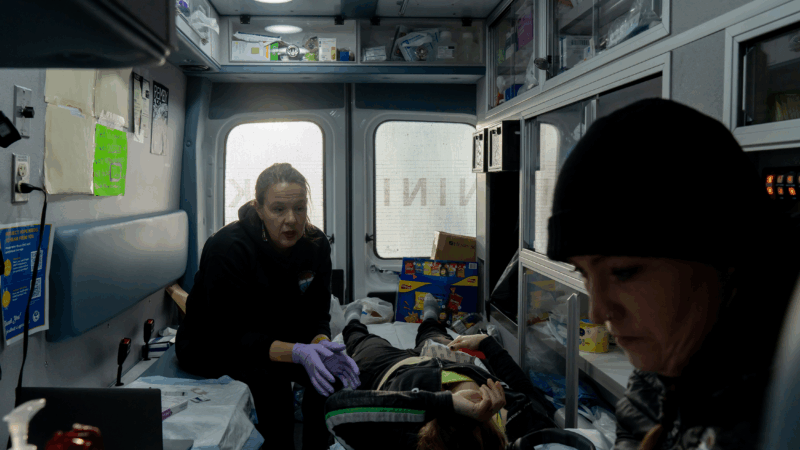
At the Ninilchik Community Clinic on Alaska’s rural Kenai peninsula this summer, Dr. Sarah Spencer stood next to a patient lying on an exam table, and swiped her belly with alcohol. The patient was there for a monthly buprenorphine shot to treat her opioid use disorder – a shot she thought might be her last for a while since there was a warrant out for her arrest. The Alaska Department of Corrections does not provide comprehensive access to this life saving medication.
“I’m gonna give you a little pinch,” Spencer said, sliding the needle into a fold of skin on the patient’s belly for the subcutaneous injection.
Alaska’s not an outlier. Despite the fact that those recently released from incarceration are some of the most vulnerable to dying from drug overdose, addiction experts say that many jails and prisons around the country don’t provide medication treatment.
Organizations like the Ninilchik Community Clinic say they do what they can to treat people going into or coming out of jail or prison, but can’t help those inside. And according to addiction medicine specialists, any interruptions in treatment could make it harder for people to stay in recovery – and survive their opioid addiction.
“I really wanted to do good”
Spencer’s patient at the clinic that day in August was a woman who asked that NPR use only her first initial, H., because she criticized the Alaska Department of Corrections and she was afraid of retaliation from staff in jail. She said she was expecting to be incarcerated for about 6 months.
H. said there are sometimes contraband drugs in jail, and she wanted to get these shots so she had the best chance of staying sober while incarcerated.
“I wanted to cover my bases, because I really, really wanted to do good,” H. said. “I didn’t want to go backwards.”
Many studies have shown that medication for opioid use disorder makes recovery more likely and reduces the risk of overdose death.
If people aren’t able to get medication while incarcerated, they may relapse in prison on black market drugs, or, if they don’t use opioids inside, they will detox and their tolerance will go down. That makes them more susceptible to overdose when they leave.
“There is no population that’s at higher risk than people who have been recently incarcerated and a big part of that is because… it only takes two weeks for people to lose their tolerance to opioids,” Spencer said.

Research backs up the idea that people sent to jails and prisons are incredibly vulnerable to drug death. Federal data released by the Biden administration showed up to 1 in 4 overdose deaths nationally in 2021 involved people “recently released from jail or prison.” And one National Institute of Health study found that in the weeks after being released from prison, people were up to 40 times more likely to die from overdoses compared with the general population.
H. said the treatment for her opioid use disorder was interrupted when she was incarcerated earlier in 2025. She said the Alaska Department of Corrections denied her medication and she started using illicit opioids again when she got out.
“It happens super fast,” H. said. “I didn’t have a phone or anything, but you run into people. You see people. It just – there’s 1,000 different ways.”
Limitations on treatment
Interviews with healthcare providers like Dr. Spencer and formerly incarcerated people like H. indicate that many who want medication while incarcerated don’t get it.
Alaska’s Department of Corrections, or DOC, declined repeated requests for an interview for this story, but they responded to questions over email.
They confirmed that they only give 30 days of medication treatment to people who were already getting it before incarceration. No one gets treatment for more than a month, unless they’re pregnant. When people are released, DOC said they give some a list of providers they can go to for treatment.
But Spencer said best practice is to make it much easier for any inmate to start and stay on medication and to provide them with a transition plan – like DOC setting up an appointment for them with a healthcare provider in the community – to help them stay safe after release.
“If a patient isn’t continued on their medication or isn’t offered medication, you’re really missing that opportunity to stabilize this life threatening disease while they’re in DOC custody,” she said.

DOC said their aim is to expand access to medication for opioid use disorder, and they hope to pilot a more comprehensive program by February of 2026.
Spencer said in the absence of comprehensive treatment, her team tries their best to provide care for people before and after incarceration, at least on the Kenai peninsula.
Her colleague Annette Hubbard is a case manager who routinely checks the court docket for active warrants – and helps those who she knows have opioid use disorder get treatment before they go in.
“I do that voluntarily, because I know that the people that I work with and for are always at risk,” Hubbard said.
A contrasting approach in Rhode Island
Spencer said she wishes Alaska’s system were more like Rhode Island’s. In 2016, the state started offering treatment for substance use disorders to anyone eligible in DOC care. Within a year, there had been a 61% reduction in overdose death rates among people recently incarcerated, and a 12% reduction in overdose deaths statewide.
Dr. Jennifer Clarke developed the program as medical director at the Rhode Island Department of Corrections.
Before she could freely dispense medication for substance use disorders, she said, “it was like practicing medicine with one hand tied behind my back.”
According to Clarke, the results of the new program were palpable: when people weren’t going through withdrawal and having cravings, they could focus better on recovery.
“I heard multiple times, people would tell me, ‘This was the first time I could really participate in the treatment classes, in the behavioral therapy,'” Clarke said.
But she said it wasn’t always easy. The program required two million dollars in funding to start, the backing of the then-governor, and it had to overcome many logistical hurdles. And she said, there was stigma.
“I was called frequently a drug pusher,” she said. “So with the medical staff, I would just talk data. I’m like, ‘We’re scientists… We’re going to follow the science.'”
Across the country, inconsistent access to care
Other states have been slow to develop similar life-saving medication programs. In a recent study published in JAMA Network Open, representative of over 3,000 U.S. jails, fewer than half offered some access to medication for opioid use disorder.
Redonna Chandler, a psychologist formerly at the National Institute on Drug Abuse, said medication can be hard to access for anyone with opioid use disorder, and often jails and prisons don’t have providers with the expertise necessary to give the medications.
“I think it’s still a patchwork of programs,” Chandler said.
And because medications like buprenorphine are opioids themselves and help alleviate symptoms of withdrawal, there are black markets for them inside jails and prisons.

“You’ll hear a lot of concerns about ‘diversion’ and about pills being diverted, but there are ways to deal with and get around that, either through other formulations or through the ways in which you would administer the medication,” Chandler said. That could mean shifting from pills to injectable formulations, which are much harder to divert.
In the meantime, some patients like H. in Ninilchik may only be able to get treatment outside incarceration.
“It would just be so huge to be able to get it in jail too, and then gain that strength to be able to help yourself when you did hit the streets again,” H. said.
It’s unclear when she will start her new jail sentence, but she said she hoped when she got out, she’d go right back to treatment. If she does, it may save her life.
Transcript:
SCOTT SIMON, HOST:
Inmates and people recently released from jails and prisons are among the most vulnerable to dying from a drug overdose. Experts say many don’t get the treatment they need. In Southcentral Alaska, one group is trying to change that, as Rachel Cassandra of Alaska Public Media reports.
SARAH SPENCER: How have you been feeling since I saw you last?
H: Pretty good.
RACHEL CASSANDRA, BYLINE: At the Ninilchik Community Clinic on Alaska’s rural Kenai Peninsula this summer, Dr. Sarah Spencer preps a patient who’s getting a monthly buprenorphine shot to treat her opioid use disorder.
SPENCER: I’m going to go on a different spot because that’s really close to your last shot, and I can feel it there.
CASSANDRA: This clinic is run by the Ninilchik Village Tribe. They serve tribal members and nontribal patients. Spencer’s patient is a woman who asks that we use only her first initial, H. She says she has a warrant out for her arrest and is expecting to go to jail for about six months. We met with H in August, and NPR agreed to identify her only by her first initial because she spoke critically of the Alaska Department of Corrections, and she’s afraid of retaliation from staff in jail.
SPENCER: OK. I’m going to give you a little pinch.
CASSANDRA: H says there are sometimes contraband drugs in jail, and she wants to get these shots so she has the best chance of staying sober while incarcerated.
H: I wanted to cover my bases because I really, really wanted to do good. I didn’t want to go backwards.
CASSANDRA: Many studies have shown that medication for opioid use disorder makes recovery more likely and reduces the risk of overdose death. If people aren’t able to get medication while incarcerated, they may relapse in prison on black market drugs. Or if they don’t use opioids inside, they will detox and their tolerance will go down. That makes them more susceptible to overdose when they leave.
SPENCER: There is no population that’s at higher risk than people who have been recently incarcerated. And a big part of that is because it only takes two weeks for people to lose their tolerance to opioids.
CASSANDRA: Research backs up the idea that people sent to jails and prisons are incredibly vulnerable to drug death. Federal data released by the Biden administration showed up to 1 in 4 overdose deaths nationally in 2021 involve people recently released from jail or prison. H says the treatment for her opioid addiction was interrupted when she was incarcerated earlier this year. She says the Alaska Department of Corrections denied her medication and that she started using illicit opioids again when she got out.
H: It happens superfast. You run into people. You see people. It’s just – there’s a thousand different ways.
CASSANDRA: Interviews with health care providers like Dr. Spencer and formerly incarcerated people like H indicate that many who want medication while incarcerated don’t get it. Alaska’s Department of Corrections, or DOC, declined repeated requests for an interview for this story, but they responded to questions over email. They confirmed that they only give short-term medication treatment to people who were already getting it before they went to jail or prison and said that no one gets treatment past 30 days unless they’re pregnant. When they’re released, DOC says they give some people a list of providers they can go to for treatment. But Spencer says best practice is to make it much easier for every inmate to start on medication and to provide them with a transition plan to help them stay safe after release.
SPENCER: If a patient isn’t continued on their medication or isn’t offered medication, you’re really missing that opportunity to stabilize this life-threatening disease while they’re in DOC custody.
CASSANDRA: DOC says their aim is to expand access, and they hope to pilot a more comprehensive program by February of 2026. Spencer says, in the absence of comprehensive treatment, her team tries their best to provide care for local people before and after incarceration. She wishes Alaska’s system was more like Rhode Island’s.
In 2016, the state started offering treatment for substance use disorders to anyone eligible in DOC care. And within a year, there had been around a 60% reduction in overdose death rates among people recently incarcerated. Dr. Jennifer Clarke developed the program as medical director at the Rhode Island Department of Corrections. She says before she could freely dispense medication for substance use disorders…
JENNIFER CLARKE: It was like practicing medicine with one hand tied behind my back.
CASSANDRA: And she says the results of the new program were palpable. When people weren’t going through withdrawal and having cravings, they could focus better on recovery.
CLARKE: I heard multiple times – people would tell me, this was the first time I could really participate in the behavioral therapy.
CASSANDRA: But Clarke says it wasn’t always easy. The program required $2 million in funding to start, the backing of the then-governor, and it had to overcome many logistical hurdles. And she says there was stigma.
CLARKE: I was called, frequently, a drug pusher. So with the medical staff, I would just talk data. I’m like, we’re scientists. We’re going to follow the science.
CASSANDRA: Other states have been slow to develop similar lifesaving medication programs. In a recent JAMA study representing over 3,000 U.S. jails, fewer than half offered some access to medication for opioid use disorder.
REDONNA CHANDLER: I think it’s still a patchwork of programs.
CASSANDRA: That’s Redonna Chandler, a psychologist formerly at the National Institute on Drug Abuse. She says medication can be hard to access for anyone with opioid use disorder. And often, jails and prisons don’t have providers with the expertise necessary to give the medications. And because medications like buprenorphine are opioids themselves and help alleviate symptoms of withdrawal, there are black markets inside jails and prisons.
CHANDLER: You’ll hear a lot of concerns about diversion and about pills being diverted. But there are ways to deal with and get around that, either through other formulations or through the ways in which you would administer the medication.
CASSANDRA: In the meantime, some patients, like H in Ninilchik, may only be able to get treatment outside incarceration.
H: It would just be so huge to be able to get it in jail, too, and then gain that strength to be able to help yourself when you did hit the streets again.
CASSANDRA: She says it’s really scary that people leaving incarceration die of overdose at such high rates. She’s thankful she survived last time, even though she returned to use. It’s unclear when H will start her new jail sentence, but she hopes this time when she gets out, with the help of the clinic, she’ll go right back to treatment. If she does, it may save her life.
For NPR News, I’m Rachel Cassandra in Ninilchik, Alaska.
Chicagoans pay respects to Jesse Jackson as cross-country memorial services begin
Memorial services for the Rev. Jesse Jackson Sr. to honor his long civil rights legacy begin in Chicago. Events will also take place in Washington, D.C., and South Carolina, where he was born and began his activism.
In reversal, Warner Bros. jilts Netflix for Paramount
Warner Bros. says Paramount's sweetened bid to buy the whole company is "superior" to an $83 billion deal it struck with Netflix for just its streaming services, studios, and intellectual property.
Trump’s ballroom project can continue for now, court says
A US District Judge denied a preservation group's effort to put a pause on construction
NASA lost a lunar spacecraft one day after launch. A new report details what went wrong
Why did a $72 million mission to study water on the moon fail so soon after launch? A new NASA report has the answer.
Columbia student detained by ICE is abruptly released after Mamdani meets with Trump
Hours after the student was taken into custody in her campus apartment, she was released, after New York City Mayor Zohran Mamdani expressed concerns about the arrest to President Trump.
These major issues have brought together Democrats and Republicans in states
Across the country, Republicans and Democrats have found bipartisan agreement on regulating artificial intelligence and data centers. But it's not just big tech aligning the two parties.